Translate this page into:
Anesthetic management of a child with a laryngeal mass associated with Laryngo-onycho-cutaneous syndrome
*Corresponding author: Mridul Dua, Department of Paediatric Anesthesiology, Bai Jerbai Wadia Hospital for Children, Mumbai, Maharashtra, India. mridul.dua@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dua M, Shikhare M, Kurup B, Sawant PH. Anesthetic management of a child with a laryngeal mass associated with Laryngoonycho-cutaneous syndrome. Wadia J Women Child Health. 2024;3(1):46-9. doi: 10.25259/WJWCH_51_2023
Abstract
With fewer than 50 reported cases, Laryngo-onycho-cutaneous syndrome is a rare condition presenting in childhood with skin and conjunctival ulcerations and laryngeal pathology. A 4-year-old girl presented with recent onset aphonia. Airway endoscopy revealed a laryngeal mass. Tracheostomy was advised but parents denied consent. Two weeks later, she developed severe stridor warranting emergent tracheostomy. The child was diagnosed as Laryngo-onycho-cutaneous syndrome, also known as Shabbir syndrome. Subsequently, she was taken up for laser excision of the mass. Here, we describe the anesthetic management in such airway procedures. Total intravenous anesthesia and local anesthetic in the form of vocal cord spray are safe and environment-friendly alternatives to inhalational anesthesia for airway endoscopies.
Keywords
Laryngeal mass
Shabbir syndrome
Airway endoscopy
Total intravenous anesthesia
Laser surgery
INTRODUCTION
In 1986, Professor Syed Ghulam Shabbir described a rare sub-type of junctional epidermolysis bullosa.[1] Laryngo-onycho-cutaneous, or Shabbir syndrome, this autosomal recessive inherited disorder is characterized by the development of vascular granulation and ulceration over the skin, conjunctiva, nails, and mucous membranes, starting in infancy [Figure 1]. Of special interest to pediatric anesthesiologists and otolaryngologists are the peculiar, and commonly life-threatening laryngeal lesions such as glottic masses, webs, and stenoses, associated with this syndrome.
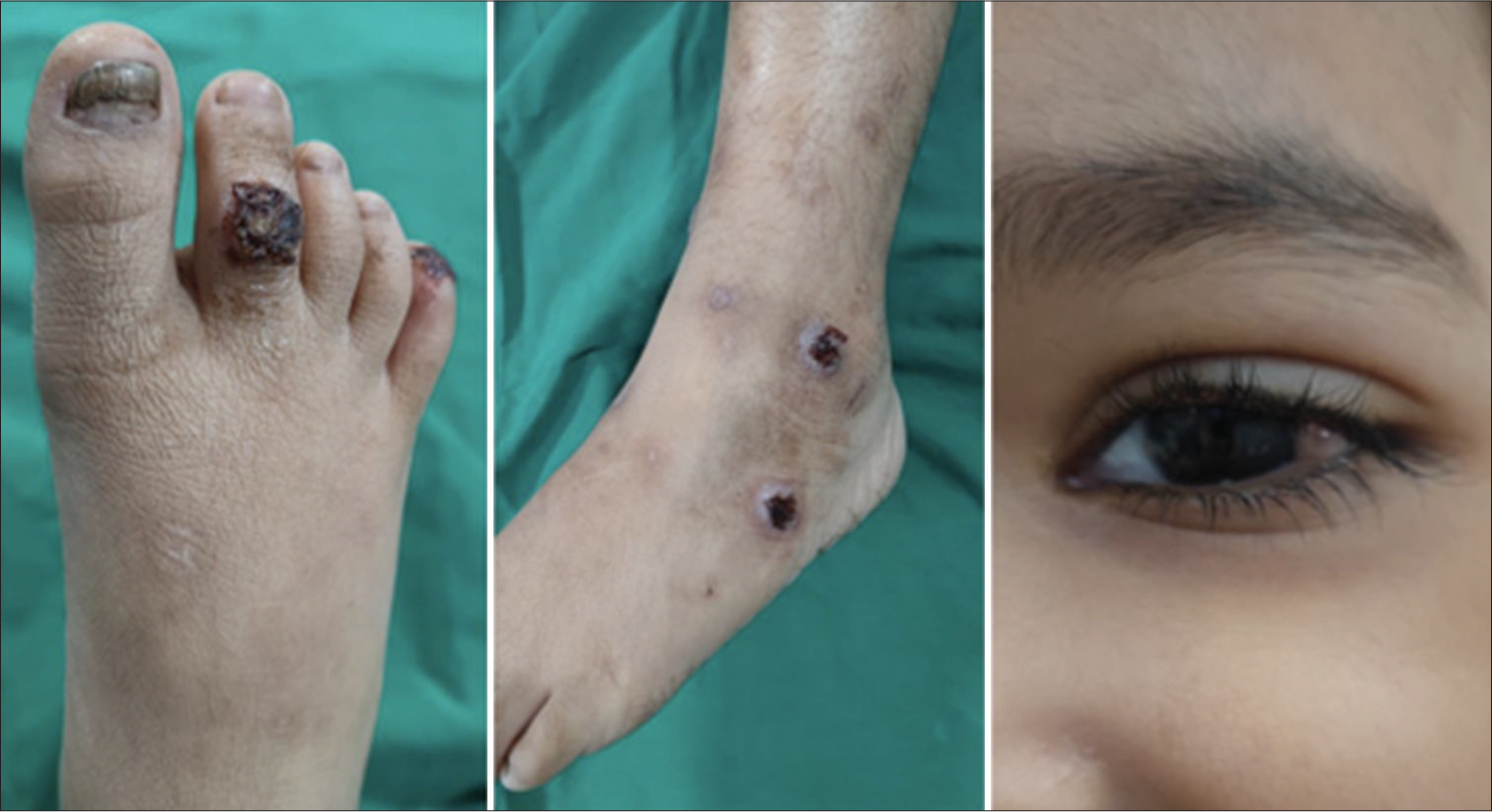
- Skin and ocular lesions in our patient with Shabbir syndrome.
Literature review revealed fewer than 50 reported cases and just two other case reports describe the anesthetic management of Shabbir syndrome.[2,3] We present the anesthetic challenges and management of a child with airway obstruction, which was later diagnosed as Laryngo-onycho-cutaneous syndrome.
CASE REPORT
A 4-year-old girl weighing 12 kgs, was brought to our hospital with aphonia since 2 weeks. An airway evaluation under general anesthesia was planned. A thorough pre-anesthetic check-up was done. Her systemic examination and blood work-up were unremarkable. She had a few crusted skin lesions over her elbows, toes, ankle, and knees, which were thought to be insignificant at the time of initial evaluation [Figure 1]. Requisite consents were taken, intravenous (IV) access was secured in the ward and she was shifted to the operating room after adequate fasting. In the operation theater, standard monitors were applied, and vitals were recorded. Baseline oxygen saturation was 100%. The ear, nose, and throat (ENT) surgeon performed an awake flexible fiber-optic bronchoscopy which revealed a laryngeal mass. The findings was to be confirmed using a Zero Degree Hopkins Endoscope, for which anesthesia was required.
We planned to employ a total intravenous anesthesia (TIVA) technique with IV propofol sedation, check for bag and mask ventilation, perform a conventional laryngoscopy, topicalize the airway with 1% lignocaine + adrenaline solution, and maintain spontaneous ventilation throughout. Oxygen was delivered using an insufflation technique, holding Jackson– Rees circuit with a flow rate of 15 L/min, near the patient’s nose. IV dexamethasone was given to prevent airway edema.
Airway assessment confirmed a 7 × 7 mm posterior glottic mass, arising from the right arytenoid [Figure 2]. The glottic opening allowed a 4.5 uncuffed endotracheal tube (ETT) to pass, and a biopsy was taken from the mass. There was minimal bleeding. The patient was shifted to the pediatric intensive care unit and electively ventilated for a day. Parents were counseled regarding the need for an elective tracheostomy until biopsy results were obtained and final treatment was planned; but they denied consent and took the child home, against medical advice.
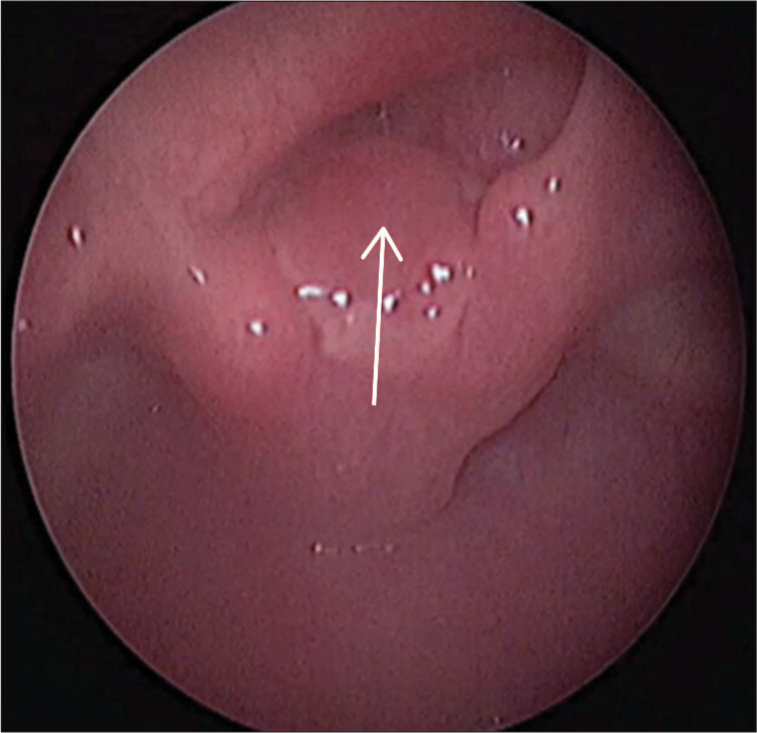
- Bronchoscopic image of the laryngeal mass in our patient (shown by arrow).
Two weeks later, the patient was brought to the Emergency room, with severe stridor. Emergency tracheostomy under general anesthesia with IV midazolam, ketamine, and propofol, was performed. Bag and mask ventilation was satisfactory, and the airway was secured with a size 2.0 i-gel® supraglottic airway device. Oxygen saturation was maintained throughout. After a successful surgical tracheostomy, the patient was sedated, paralyzed, and electively ventilated for 48 hours.
The parents refused further evaluation by dermatologist and ophthalmologist. Six weeks later, follow-up airway assessment was done under TIVA with ventilation through the tracheostomy tube, which revealed an increase in the size of the laryngeal mass and anterior glottic membranous web with complete occlusion of glottic inlet. Skin and nail ulcers had increased in size and number, and small granulomatous lesions had developed in bilateral conjunctivae. Opinion from a pediatric rheumatologist was sought, and a definitive diagnosis of Laryngo-onycho-cutaneous syndrome was made. Laser excision of the laryngeal mass and web was planned, with a need for close and regular follow-up.
Three months later, CO2 laser excision of the mass and web was done using a suspension microlaryngoscope. We employed a TIVA technique with propofol (100–150 mcg/kg/min), dexmedetomidine (0.5 mcg/kg/h), and atracurium (0.5 mg/kg/h) infusions. The airway was anesthetized using 1% lignocaine + adrenaline spray, under direct laryngoscopy. The patient was ventilated through the tracheostomy tube with an air-oxygen mixture, 20–30% FiO2, with intermittent apnea. The face and head were wrapped with wet mops to prevent airway fire [Figure 3].

- Head and face wrapped with wet mops for laser airway surgery under suspension microlaryngoscope.
The mass and web were excised, and a laryngeal stent was fashioned using a 4.5 size silicone nasopharyngeal airway. The procedure lasted 3 hours, anesthesia was reversed, and the child was shifted to the recovery room on oxygen through tracheostomy tube.
DISCUSSION
When it comes to rare diseases, there is a lack of consensus and guidelines on their anesthetic management. Through this article, we aim to shed light on the challenges that a patient with Shabbir syndrome or any glottic mass, presents.
The constellation of signs and symptoms in Shabbir syndrome include:[4,5]
Periungual hypergranulation
Skin fragility, crusted ulcers
Conjunctival and corneal ulcerations
Symblepharon or total palpebral occlusion
Blindness
Laryngeal masses, webs, and stenosi
Aphonia
Respiratory obstruction
Enamel hypoplasia and dental malformations
Most patients have a poor prognosis, due to skin and respiratory infections or respiratory obstruction. Surgical interventions such as tracheostomy, gastrostomy, and suprapubic catheterizations may be required to avoid strictures and stenoses during the first decade of life. Few survivors have required lifelong tracheostomy, and some cases have shown remission in the second decade of life.[6]
The lesions are usually refractory to pharmacotherapy, but some antibiotics, thalidomide, dapsone, and steroids have shown positive results.[6] Laser excision of laryngeal masses has been attempted by some.[2] In one report, topical Mitomycin C was successfully used to treat an 18-year-old patient with laryngeal stenosis with Shabbir syndrome.[7]
Our patient had all the classic lesions of Laryngo-onycho-cutaneous syndrome, but the unwillingness of the parents to get the necessary management not only caused delay in diagnosis but also caused a life threatening risk to the child.
When anesthetising a pediatric patient with suspected airway obstruction, the anesthetist must ensure the presence of a peripheral venous line placed pre-induction. The risk of life-threatening respiratory obstruction during inhalational induction outweighs the fear and pain that the child might experience due to awake IV cannulation.
Anesthesia for airway endoscopy and laryngeal surgeries poses a plethora of unique challenges. Both surgeons and anesthesiologists are working in the same anatomical location. The anesthesiologist must keep the child still, maintain a patent airway, and prevent aspiration, laryngospasm and hemodynamic instability. In addition, the pediatric anesthesiologist needs to have alternative management plans given that these procedures are often dynamic and sometimes unpredictable, e.g., patients may initially maintain adequate spontaneous ventilation but later become apneic, necessitating intervention and alterations in the previously developed plan.[8]
One can opt for TIVA or inhalational anesthesia with sevoflurane or a combination of both techniques. Inhalational anesthesia with spontaneous respiration is traditionally used to facilitate airway endoscopy in children. The potential difficulties in maintaining an adequate depth of anesthesia using inhalational anesthesia and the anesthetic pollution of the surgical environment are significant disadvantages of this technique. Malherbe et al report the use propofol and remifentanil infusions and a TIVA technique in over 50 airway endoscopies.[9]
The authors prefer using TIVA for all airway procedures, propofol being the drug of choice. Propofol is carefully titrated to keep the child sedated and still allow the procedure while maintaining spontaneous respiration. During airway endoscopy under anesthesia, oxygenating a child with upper airway obstruction and laryngeal pathology can be particularly demanding. Our practice is to keep the patient-end of the circuit near the child’s nose and increase oxygen flows to 15 L/min and give continuous positive airway pressure (CPAP) to the anesthetized, spontaneously breathing child.
In addition, for bronchoscopy, we topicalize the airway and spray the vocal cords and glottic structures with 1% lignocaine + adrenaline solution under direct laryngoscopy using a 2 mL Luer lock syringe to avoid needle dislodgment. This method of topicalizing the vocal cords, while simple, is extremely effective and prevents catastrophic airway obstruction due to laryngospasm.
Laser procedures pose risks to the patient and medical personnel. Surgical fires are rare, but potentially catastrophic events, most of which occur during head and neck surgery.[10] Of the three elements necessary for fire ignition, all exist during airway cases: An oxidizer (oxygen), a fuel (sponges and ETTs), and an ignition source (lasers and electrocautery). During airway cases using cautery or laser, the anesthesiologist may reduce the FiO2 to <30% to reduce risk.
Most importantly, constant active and clear communication between the ENT surgeon and anesthesiologist is crucial for successful outcomes in such patients.
CONCLUSION
This article reports a rare case of Laryngo-onycho-cutaneous syndrome in a pediatric patient. While the prognosis remains guarded, this report can serve as an example of the anesthetic management strategy for a child who presents with this dreadful condition. Early tracheostomy and routine follow-ups are essential and form the mainstay of management.
In addition, a TIVA technique for airway surgeries, with topicalization of the glottic structures with lignocaine + adrenaline, under direct laryngoscopy is helpful. We believe this technique is superior to inhalational anesthesia as we can maintain a steady plane of anesthesia with titrated doses of propofol, without contaminating the operating room with sevoflurane.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anaesthesia for airway obstruction in laryngo-onycho-cutaneous syndrome. Anaesthesia. 1993;48:503-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anaesthetic management of a child with laryngo-onycho-cutaneous syndrome. Anaesth Cases. 2014;2:3-7.
- [CrossRef] [Google Scholar]
- Multisystem disorder of Punjabi children exhibiting spontaneous dermal and submucosal granulation tissue formation: LOGIC syndrome. Clin Dysmorphol. 1992;1:3-15.
- [CrossRef] [PubMed] [Google Scholar]
- The natural history of laryngo onycho-cutaneous syndrome: A case series of six pediatric patients and literature review. Pediatr Dermatol. 2021;38:1094-101.
- [CrossRef] [PubMed] [Google Scholar]
- Laryngo-onychocutaneous syndrome. Dermatol Clin. 2010;28:89-92.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of laryngeal stenosis in laryngo-onycho-cutaneous syndrome with topical mitomycin C. Pediatr Dermatol. 2006;23:75-7.
- [CrossRef] [PubMed] [Google Scholar]
- Anesthesia methods for airway endoscopy In: Anesthetic management for the pediatric airway: Advanced approaches and techniques. Germany: Springer; 2019. p. :43-57.
- [CrossRef] [Google Scholar]
- Total intravenous anesthesia and spontaneous respiration for airway endoscopy in children-a prospective evaluation. Pediatr Anesth. 2010;20:434-8.
- [CrossRef] [PubMed] [Google Scholar]






