Translate this page into:
Childhood pilomatrixoma: Case series with a comprehensive literature review
*Corresponding author: Arka Banerjee, Department of Pediatric Surgery, Bai Jerbai Wadia Hospital for Children, Mumbai, Maharashtra, India. arkabanerjee6989@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tiwari YA, Banerjee A, Patwardhan LM, Bendre P. Childhood pilomatrixoma: Case series with a comprehensive literature review. Wadia J Women Child Health 2023;2(2):70-2.
Abstract
Pilomatrixoma is a benign skin tumor that develops from the hair follicle matrix cells. It represents around 0.1% of all skin tumors. Although pilomatrixomas are well-recognized lesions, clinically they are frequently misdiagnosed primarily due to a lack of awareness by clinicians. We have retrospectively reviewed medical records of six children with a histologically diagnosed pilomatrixoma between January 2018 and April 2023. There were four boys and two girls with median age at presentation of 8 (range 4 to 12) years. The common complaint was of a painless swelling that was immobile and fixed to the overlying skin. All but one patient had solitary lesions and most of them were in the head and neck region. The size of the lesions ranged from 0.8 to 1.5 cm. All the patients had their lesions excised completely and sent for histopathological examination which confirmed the diagnosis of a pilomatrixoma. After a median follow-up of 16 (range 12 to 47) months, none of our patients developed any recurrence or malignancy. Pilomatrixoma is an uncommon benign skin tumor, sometimes with atypical forms, with no tumor-specific diagnostic feature except for a careful histopathological examination. It is easily excisable and recurrence is rare.
Keywords
Pilomatrixoma
Pilomatricoma
Calcifying epithelioma
INTRODUCTION
Pilomatrixoma (or “pilomatricoma”) is a benign skin tumor that develops from the hair follicle matrix cells. First described as a calcifying epithelioma of sebaceous glands by Malherbe and Chenantois in 1880, it was named “pilomatrixoma” by Forbis and Helwig in 1961 revealing the cortex of the follicle as the site of origin.[1] Pilomatrixoma represents around 0.1% of all skin tumors.[2] Although pilomatrixomas are well-recognized lesions, clinically they are frequently misdiagnosed probably due to a possible lack of awareness of this tumor.[3] We present a series of six cases of pediatric pilomatrixomas to increase awareness and also, avoid misdiagnoses of pilomatrixomas in children.
CLINICAL PRESENTATION
The medical records of six children with histologically diagnosed pilomatrixoma at the pediatric surgery department of our institute, between January 2018 and April 2023, were retrospectively evaluated. The patients’ medical history, radiological details, and histopathology reports were analyzed and they were followed up for recurrence or malignant transformations. Table 1 summarizes the clinical features. There were four boys and two girls with a median age at presentation of 8 (range 4 to 12) years.
| Age (years) | Sex | Site | Number | Maximum dimension (cm) | Follow-up (months) |
|---|---|---|---|---|---|
| 4 | M | Pre-auricular | 1 | 1.0 | 56 |
| 10 | F | Axilla | 1 | 1.5 | 47 |
| 8 | M | Neck | 1 | 1.5 | 18 |
| 4 | F | Neck | 2 | 0.8 | 14 |
| 12 | M | Neck | 1 | 1.5 | 12 |
| 8 | M | Neck | 1 | 1.5 | 7 |
These children were admitted with complaints of painless swelling at the site of lesion. One patient had two lesions and the rest had solitary lesions. Except for one child with an axillary pilomatrixoma, all had lesions in the head and neck region [Table 1]. The swellings were painless, immobile, and fixed to the overlying skin [Figure 1]. The size of the lesions ranged from 0.8 to 1.5 cm. All the lesions were excised completely.
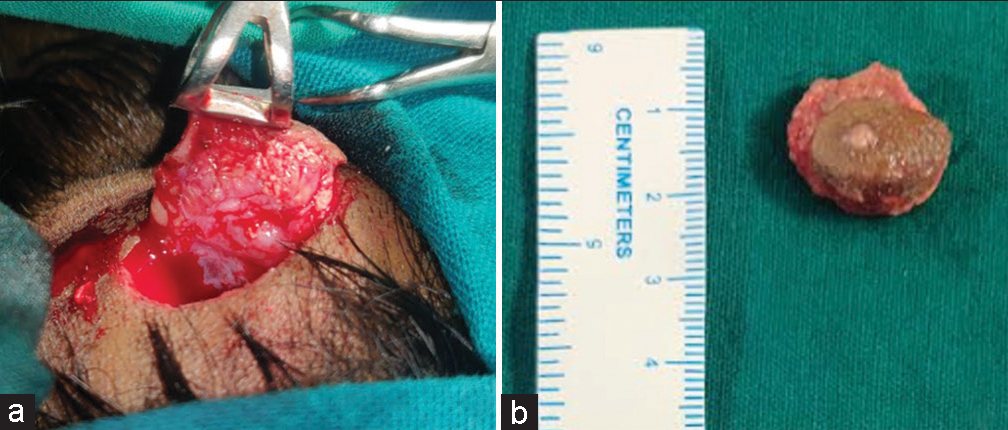
- (a) Intra-operative picture and (b) excised specimen with overlying skin showing no discernible clinical feature from a sebaceous cyst.
Histopathology revealed evidence of pilomatrixoma [Figures 2 and 3] which included basaloid proliferation of cells maturing into anucleate ghost cells, foreign body giant cells along with lymphocytes and histiocytes, and foci of calcification. During the median follow-up of 16 (range 12 to 47) months, none of our patients developed a recurrence or a malignancy.
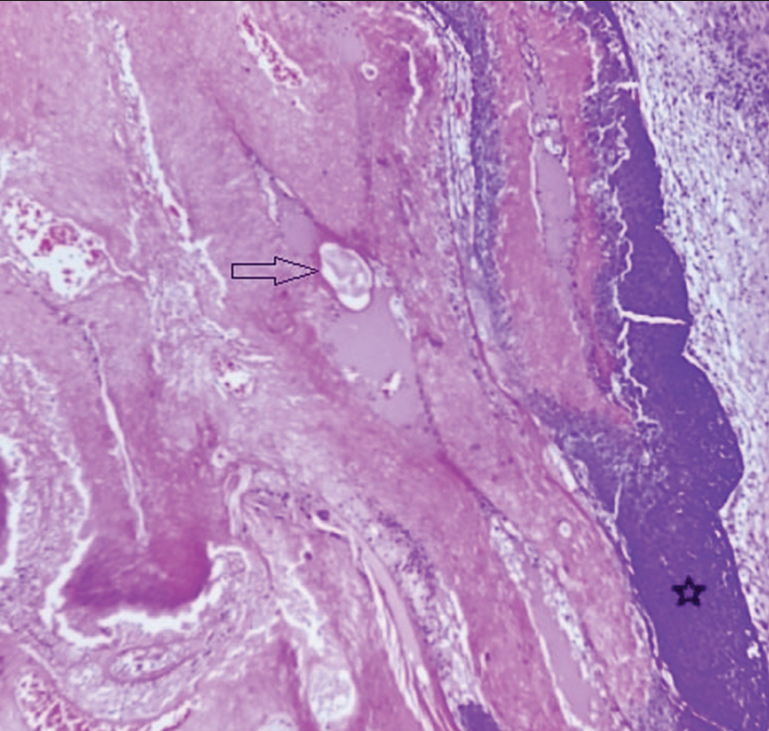
- Anucleate squamous cells (Ghost cells; light arrow), basaloid cell cluster with foci of calcification (asterisk) (H&E, ×100 magnification).
![Foreign body-type multinucleated giant cells (dark arrow) [H&E, ×100 magnification].](/content/147/2023/2/2/img/WJWCH-2-070-g003.png)
- Foreign body-type multinucleated giant cells (dark arrow) [H&E, ×100 magnification].
DISCUSSION
Pilomatrixoma is the second-most common benign skin tumor of childhood,[4] seen commonly in hairy regions, most frequently in the head and neck (64%), upper extremities (22%), trunk (8%), and lower extremities (5%).[1,5] The etiology is unclear but is thought to be due to a pause in the life cycle of hair follicles due to trauma and/or inflammation.[6] Polyomavirus has also been reported as a causative agent.[7]
With a peak incidence between 8 and 10 years of age, 60% of patients are under 20-years-old with a female preponderance of 1.5–2.06 times.[8] About 75% of patients have a 3p22-p21.3 gene locus β-catenin mutation.[6] Known associations are with Gardner’s syndrome, myotonic muscular dystrophy, Turner syndrome, skull dysostoses, sarcoidosis, and Rubinstein-Taybi syndrome.[8,9]
The common presentation is of a firm, slowly growing, and immobile nodule. They are usually asymptomatic but can be painful in case of inflammation and ulceration.[1,10] The tumoral calcifications, by excessive tension, may cause the skin to appear conical in shape, seen as a hard calcified nodule. The lesion is usually single, but 8.2–33.3% have multiple pilomatrixomas.[11] Multiple tumors may be associated with a positive familial history[12] or hypercalcemia.[13] Except in rare cases, development is generally slow over months to years.[14]
The reported diagnostic accuracy of pilomatrixoma by ultrasonography is 13.3%.[15] It is seen as internal reticulations on a hypoechoic background with or without a hypoechoic rim that represents the capsule of the pilomatrixoma. Doppler shows vascularity in 50–70% of childhood pilomatrixomas.
On histopathological examination, a keratin core at the center of the lesion surrounded by peripheral basophilic (basaloid) cells is seen (“shadow” or “ghost” cells) which are pathognomonic for pilomatrixoma. In addition, foreign body reactions are seen in 83%, stromal hemosiderin pigment in 25%, and ossification in 15–20% of cases.[2]
Treatment is total surgical excision and biopsy is confirmatory. Recurrence is rare, seen in <3% of cases. Although almost all pilomatrixomas are benign, malignant transformations are rarely noted and metastases to the lungs, bone, brain, and skin have also been reported.[16] The incidence of pilomatrix carcinoma increases in older age and is 3 times more common in men at an average age of affection around 44 years. Features suggestive of malignancy include ulceration, nuclear pleomorphism, atypical mitosis, central necrosis, and/or infiltration of the skin or adjacent tissues.[4] For treatment of the malignant form, excision with a 1–2 cm safety margin is recommended. However, adjuvant chemotherapy with or without radiotherapy is also advisable.
CONCLUSION
Pilomatrixoma is an uncommon benign skin tumor, sometimes with atypical forms. However, it is treatable with a simple surgical excision, and long-term clinical follow-up is adequate to detect any recurrence or malignant transformation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Pilomatrixoma (calcifying epithelioma). A statistical study. Arch Dermatol. 1973;108:532-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma--accuracy of clinical diagnosis. J Pediatr Surg. 2006;41:1755-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma in the head and neck. Braz J Otorhinolaryngol. 2009;75:618.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma: A comprehensive review of the literature. Am J Dermatopathol. 2018;40:631-41.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma: A review of 346 cases. Plast Reconstr Surg. 2003;112:1784-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rapidly growing pilomatrixoma on eyebrow. Indian J Ophthalmol. 2008;56:83-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma of the head and neck in six cases. Kulak Burun Bogaz Ihtis Derg. 2005;14:121-6.
- [Google Scholar]
- Childhood pilomatrixoma: Case series from a single center. Trends Pediatr. 2020;1:39-43.
- [CrossRef] [Google Scholar]
- Head and neck pilomatricoma in the pediatric age group: A retrospective study and literature review. Int J Pediatr Otorhinolaryngol. 2001;57:123-8.
- [CrossRef] [PubMed] [Google Scholar]
- Giant pilomatrixoma (benign calcifying epithelioma of Malherbe) of the neck and face. Dermatol Surg. 2007;33:340-3.
- [CrossRef] [PubMed] [Google Scholar]
- Review of pediatric head and neck pilomatrixoma. Int J Pediatr Otorhinolaryngol. 2016;85:148-53.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple familial pilomatricomas: An unusual case. J Cutan Pathol. 2004;31:281-3.
- [CrossRef] [PubMed] [Google Scholar]
- Eyelid pilomatrixoma: A description of 16 cases and a review of the literature. Surv Ophthalmol. 2008;53:526-35.
- [CrossRef] [PubMed] [Google Scholar]
- Large, rapidly growing pilomatrixoma of the upper eyelid. Ophthalmic Plast Reconstr Surg. 2006;22:401-3.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatricoma of childhood: A common pathologic diagnosis yet a rare radiologic one. Am J Roentgenol. 2016;206:182-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pilomatrixoma in childhood. J Cancer Res Therapeutics. 2014;10:549-51.
- [CrossRef] [PubMed] [Google Scholar]






