Translate this page into:
Mystifying joint pains: Acute lymphoblastic leukemia presenting as systemic onset juvenile idiopathic arthritis
*Corresponding author: Ritika Khurana, Department of Pediatric Hematology - Oncology, Bai Jerbai Wadia Hospital for Children, Parel, Mumbai, Maharashtra, India. ritangel247@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khurana R, Kanvinde P, Chadha V, Krishnan VP, Patel S, Sharma AN et al. Mystifying joint pains: Acute lymphoblastic leukemia presenting as systemic onset juvenile idiopathic arthritis. Wadia J Women Child Health 2022;1(2):67-71.
Abstract
Objectives:
Acute Lymphoblastic Leukemia (ALL) in children presents with varied manifestations. At times, they may mimic symptoms and signs of Systemic onset Juvenile Idiopathic Arthritis (SoJIA). We analyzed children with ALL who were initially diagnosed as SoJIA thus leading to delay in diagnosis and treatment of ALL.
Material and Methods:
Retrospective study of records of 18 children diagnosed as ALL at our center between the period of January 2016 and December 2020, and who were initially diagnosed as SoJIA.
Results:
All 18 children presented with fever and joint pains involving large joints such as knee, ankle, wrist, and elbow. Seven (38.8%) cases had associated hepatosplenomegaly and three (16%) had lymphadenopathy at the time of presentation. Ten out of 18 children (55.6%) had normal peripheral complete blood counts. The duration from the time of onset of symptoms to diagnosis of ALL ranged from 15 days to 7 months in these cases. Four children had received steroids as treatment of SoJIA before they were diagnosed with ALL.
Conclusion:
Possibility of ALL must be ruled out in all cases suspected of having SoJIA, as leukemias may not always present with typical signs like hepatosplenomegaly, lymphadenopathy, or cytopenias. It will prevent delay in diagnosis and treatment of ALL. Administration of steroids to these patients for SoJIA, adversely affects post-ALL treatment outcomes.
Keywords
Acute lymphocytic leukemia
Systemic onset Juvenile idiopathic arthritis
Arthralgia
Leukemia
Bone marrow aspiration
Steroids
INTRODUCTION
Acute Lymphoblastic Leukemia (ALL) is the most common pediatric cancer. It commonly presents with fever, pallor, skin or mucosal bleeding, organomegaly and cytopenia.[1] Some of the patients present with arthralgia (joint pain) or overt arthritis (localized joint swelling, redness, and restriction of motion). Musculoskeletal symptoms were seen in 18.5% of the patients with ALL in one of the previous studies.[2] Systemic-onset Juvenile Idiopathic Arthritis (SoJIA) has been defined as a subtype of Juvenile Idiopathic Arthritis (JIA) and characterized by six weeks of arthritis accompanied by intermittent fever either daily or twice daily for at least two weeks, in children aged less than 16 years of age, without any underlying identifiable etiology.[3] Jones et al. compared leukemia versus JIA patients and demonstrated a high sensitivity and specificity of the combination of hematological abnormalities and night time pain for making a diagnosis of leukemia.[4] This study was undertaken to determine the proportion of ALL patients who were initially labeled as SoJIA but later turned out to be leukemia. We also aimed to assess the clinical features and laboratory parameters that point towards leukemia over SoJIA in a child with musculoskeletal pains.
MATERIAL AND METHODS
Records of all children with ALL diagnosed between January 2016 and December 2020 were reviewed. All cases who were being evaluated and/or treated as SoJIA in view of predominant musculoskeletal symptoms were included in this study. Patient records of 18 children who fulfilled the study criteria were reviewed in this retrospective, analytical, and cross-sectional study. Details including age of onset of symptoms, age at presentation to our hemato-oncology services, gender, chief presenting complaints including details of pain, the site, severity, diurnal variation, any swelling of joints, constitutional symptoms such as fever, rash or weight loss, presence of pallor, petechiae, lymphadenopathy, and hepatosplenomegaly were noted. Diffuse pain in both legs was classified as leg pains and pain distinctly localized to one or more joints as arthralgia. The presence of joint swelling with or without redness and restriction of motion was defined as arthritis. Children with arthralgia and/or arthritis were considered to have joint involvement. Treatment received before presentation was also noted.
Details of laboratory evaluation, including complete blood count (CBC) were analyzed. Anemia was defined as Hb <10 g%; leukopenia as Total Leukocyte Count (TLC) <4 × 109/L, leukocytosis as TLC >12 × 109/L, neutropenia as absolute neutrophil count <1 × 109/L, thrombocytopenia as platelets <100 × 109/L, markers of increased cell turnover such as serum lactate dehydrogenase (LDH) >450 IU/L and uric acid >7 g%, were also recorded. ALL was diagnosed based on flow cytometry of peripheral blood/bone marrow sample. The presence of blast population of more than 20% was considered as ALL. Cytogenetics testing was done by FISH (Fluoresence in Situ Hybridization) and ploidy analysis.
The time lag between onset of symptoms and diagnosis of ALL was noted and any history of treatment received for SoJIA was also noted.
Disease evaluation was done post-completion of induction chemotherapy by measuring minimal residual disease (MRD) by flow cytometry. MRD of more than 0.01% was considered positive and a marker of high risk.
RESULTS
Of the 354 children diagnosed with ALL during the study period (January 2016–December 2020), 298 were Pre B ALL and 56 were T ALL. Amongst them, 18 children (5%) (all were PreB ALL) presented with predominant musculoskeletal symptoms and hence were labeled as JIA or SoJIA. Thirteen of them were males and five were females. Age at presentation ranged from 3 to 13 years with median age at presentation of 5.5 years.
Children with arthralgia and/or arthritis were considered to have joint involvement. Most common joints involved were large joints such as knee, ankle, elbow, and wrists. Fever was present in 13 (72%) cases at the onset and was associated with joint pains. Other typical features of ALL such as hepatosplenomegaly, was present in 7/18 (38.8%) and lymphadenopathy in 3/18 (16%) cases. Ten out of 18 children (55.6%) did not have any cytopenias at presentation [Figure 1]. LDH was increased in 13/18 (72%) and uric acid was increased in 2/18 (11%) cases. Initial suspicion of SoJIA led to a lag period of 15 days to 7 months (mean of 80 days) between onset of symptoms and diagnosis of ALL. Six patients (33.3%) had received steroids before the diagnosis of ALL. [Table 1] One of the patient also received weekly methotrexate for two months as a second line treatment for JIA before he was diagnosed with ALL. One patient was provisionally diagnosed as post-COVID Multisystem Inflammatory Syndrome-Children (MIS-C) and twice treated with courses of steroids but later turned out to be ALL.
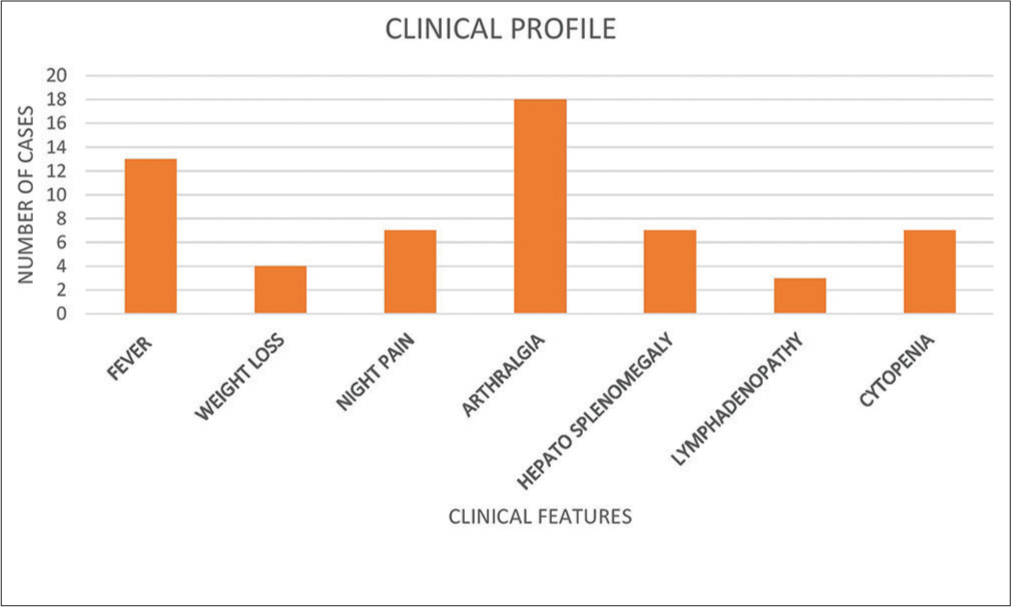
- Common symptoms and signs in children with acute lymphoblastic leukemia initially diagnosed as Systemic onset Juvenile Idiopathic Arthritis.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 9 | 3 | 9 | 7 | 3 | 7 | 4 | 5 | 7 | 5 | 6 | 13 | 8 | 12 | 3 | 9 | 3 | 3 |
| Sex | F | F | M | M | M | M | M | F | M | M | M | M | M | M | M | M | F | M |
| Constitutional Symptoms | ||||||||||||||||||
| Fever | Yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | no | no | no | no | yes | yes | yes | yes |
| Weight loss | no | no | no | yes | no | no | yes | yes | no | yes | no | no | no | no | yes | no | no | no |
| Rash | no | no | no | no | no | no | no | no | yes | no | no | no | no | no | no | no | no | no |
| Night pains | no | yes | yes | no | no | yes | yes | no | yes | yes | no | no | no | no | yes | no | no | no |
| Hepatomegaly | no | yes | yes | yes | yes | no | no | yes | no | no | no | no | no | no | yes | yes | no | yes |
| Lymphadenopathy | Yes | no | no | yes | no | no | no | no | yes | no | no | no | no | no | no | yes | no | no |
| Arthralgia/arthiritis | Yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes | yes |
| Time b/w onset and diagnosis (months) | 4 | 2 | 5 | 7 | 1 | 0.5 | 2 | 2 | 1 | 6 | 1.5 | 0.5 | 2 | 6 | 2 | 5 | 0.6 | 0.3 |
| Treatment received for JIA | NSAID | Steroids | Steroids | Steroids, Methotrexate | NSAID | None | None | Steroids | NSAID | NSAID | Steroids | None | NSAID | NSAID | NSAID | None | Steroids | None |
| Hematology parameters | ||||||||||||||||||
| Hb (g/dl) | 10 | 11.2 | 10 | 10.1 | 10 | 9.5 | 11.1 | 9.8 | 11.2 | 7.9 | 6.6 | 5.5 | 11.2 | 11.2 | 11.4 | 8.2 | 10.4 | 12.1 |
| TLC (cumm) | 7400 | 8280 | 12000 | 2250 | 6250 | 9580 | 7890 | 3500 | 6840 | 4200 | 4300 | 4000 | 5500 | 5500 | 14100 | 4000 | 9440 | 7200 |
| ANC | 2146 | 2815 | 1440 | 1130 | 3240 | 5364 | 4320 | 1240 | 2932 | 126 | 1548 | 2200 | 2750 | 2750 | 8178 | 2800 | 5130 | 4248 |
| ALC | 4810 | 6790 | 9840 | 1020 | 2240 | 3544 | 2980 | 2150 | 3650 | 3948 | 2623 | 1720 | 2090 | 2090 | 4371 | 1080 | 3940 | 2448 |
| Platelet (lac) | 2.38 | 1.05 | 0.12 | 0.09 | 0.65 | 2.42 | 2.67 | 0.55 | 1.64 | 1.82 | 4.55 | 1.95 | 4.62 | 4.62 | 4.58 | 0.05 | 2.65 | 4.66 |
M: Male, F: Female, b/w: between, Hb: Hemoglobin, NSAID: Non-Steriodal Anti-Inflammatory Drug, ALC: Acute Lymphocyte Count, lac: Lakhs
Most patients 17/18 (94.4%) had favorable cytogenetics at diagnosis and only one child had high risk cytogenetics (t [17,19]). Among the favorable cytogenetics, hyperdiploidy was seen in 6/18 (33.3%) and t (1,19) was present in 4/18 (22.2%) cases. MRD was positive in 6/18 (33.3%) patients and three (16.6%) from MRD positive group succumbed during treatment (two due to disease progression and one had severe sepsis). Among the 6 children with a positive MRD, four had received steroids prior to diagnosis of ALL. Out of the other two with MRD positive, one was with a very high risk cytogenetics t (17,19) and the other one had no explainable risk factors for MRD to be positive.
DISCUSSION
Leukemia is the most common childhood malignancy in many countries, including India.[5] The clinical picture of acute leukemia in children constitutes varied manifestations unlike adults. The disease may present with predominantly musculoskeletal symptoms mimicking JIA, rheumatic fever, juvenile systemic lupus erythematosus, vasculitis, and in recent times post-COVID MIS-C.
Approximately 4–41% of children and adolescents with JIA have SoJIA.[6]
International League of association for rheumatologists definition of SoJIA is as follows: [7]
Arthritis in one or more joints plus
Fever (with or preceding arthritis) of at least two weeks duration that is daily (“quotidian”) for at least three days plus
-
One or more of the following:
Evanescent (non-fixed) erythematous rash
Generalized lymph node enlargement
Hepatomegaly and/or splenomegaly
Serositis.
Exclusions include
Psoriasis or a history of psoriasis in the patient or first-degree relative.
Arthritis in an HLA-B27-positive male beginning after the sixth birthday.
Ankylosing spondylitis, enthesitis-related arthritis, sacroiliitis with inflammatory bowel disease, Reiter’s syndrome, or acute anterior uveitis, or a history of one of these disorders in a first-degree relative
The presence of IgM rheumatoid factor on at least two occasions at least three months apart.
Tamashiro et al., in 2011, compared 57 patients of ALL with musculoskeletal symptoms with 102 patients of SoJIA.[8] Our findings were similar to theirs in that limb pain, hepatomegaly, weight loss, and hemorrhagic manifestations were predominantly present in leukemia patients as compared to SoJIA. Kesarapu et al. similarly found in their study that most children with musculoskeletal symptoms along with thrombocytopenia, neutropenia and lymphocytosis turned out to be leukemia.[9]
A child with leukemia may present without any obvious abnormality in the CBC parameters or peripheral smear. Ten out of 18 (55.6%) children in this cohort had normal complete blood counts at presentation and 6/18 (33.3%) of our patients had only musculoskeletal symptoms at presentation, without organomegaly and/or cytopenias.
The prognostic significance of musculoskeletal symptoms in ALL has been a topic of debate.
Many studies had shown that the children with severe skeletal abnormalities may have an indolent form of leukemia. A study by Brix et al. found that children with joint involvement had better event-free and overall survival (OS). [2] Seventeen of our patients (94.4%) had favorable cytogenetics, suggestive of a good prognosis. In a study on 488 children by Pui et al. on impact of MRD in different types of ALL, children with ALL with Hyperdiploidy (Chromosomes >50) had Event Free Survival (EFS) of 91.3% (95% CI, 84.3–95.3) and OS of 96.8% (95% CI, 91.6–98.8). Similarly, in patients of ALL with t (1,19), EFS was 89.3% (95% CI, 70.4–96.4) and OS was 100%.[10] Four patients who had received steroids before, despite having favorable cytogenetics, had MRD positive post-induction chemotherapy. Escalation of therapy in otherwise standard risk patients makes them prone to chemotherapy related toxicities and infections. We lost two such patients during treatment (one to the disease and other to sepsis).
Recently, post-COVID MIS-C is a diagnosis that has confounding features at presentation and warrants thorough clinical examination, laboratory work up, and bone marrow examination whenever in doubt before starting steroids.
Gatineau-Sailliant et al. did a study on 11 children who received steroids (0.6–3.3 mg/kg/day prednisolone equivalent) for a duration of 2 to 15 days during the two months before diagnosis of ALL. They observed delay in diagnosis of ALL and increased complications such as steroid resistance and infections during induction therapy in these patients.[11]
CONCLUSION
Possibility of leukemia should always be considered even in the presence of normal complete blood counts in patients suspected of SoJIA. Opinion from a hemato-oncologist must be sought and bone marrow aspiration must be considered to rule out leukemia before starting steroids. Management ALL and SoJIA is long-term and challenging. Utmost care must be taken while making a diagnosis, so that right path is chosen for their treatment.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Musculoskeletal problems in pediatric acute leukemia. J Pediatr Orthop B. 2013;22:264-9.
- [CrossRef] [PubMed] [Google Scholar]
- Arthritis as presenting manifestation of acute lymphoblastic leukaemia in children. Arch Dis Child. 2015;100:821-5.
- [CrossRef] [PubMed] [Google Scholar]
- Initial manifestations and clinical course of systemic onset juvenile idiopathic arthritis: A ten-year retrospective study. J Formos Med Assoc. 2012;111:542-9.
- [CrossRef] [PubMed] [Google Scholar]
- A multicenter case-control study on predictive factors distinguishing childhood leukemia from Juvenile rheumatoid arthritis. Pediatr. 2006;117:840-4.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and pattern of childhood cancers in India: Findings from population-based cancer registries. Indian J Cancer. 2016;53:511-2.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the management of systemic juvenile idiopathic arthritis and role of IL-1 and IL-6 inhibition. Adolesc Health Med Ther. 2017;8:125-35.
- [CrossRef] [PubMed] [Google Scholar]
- Discrimination of acute lymphoblastic leukemia from systemic-onset juvenile idiopathic arthritis at disease onset. Clinics (Sao Paulo). 2011;66:1665-9.
- [Google Scholar]
- Acute leukemia presenting with musculoskeletal manifestations: A case series. Indian J Med Paediatr Oncol. 2020;41:29-33.
- [CrossRef] [Google Scholar]
- Clinical impact of minimal residual disease in children with different subtypes of acute lymphoblastic leukemia treated with Response-adapted therapy. Leukemia. 2017;31:333-9.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid intake before leukemia diagnosis impairs outcome in childhood acute lymphoblastic leukemia. Arch Pediatr. 2013;20:341-7.
- [CrossRef] [PubMed] [Google Scholar]






