Translate this page into:
Role of peripartum cesarean section in maternal collapse in pregnancy
*Corresponding author: Geetha Dharmesh Balsarkar, Department of Obstetrics and Gynecology, Nowrosjee Wadia Maternity Hospital, Seth G.S. Medical College, Mumbai, Maharashtra, India. gdbalsarkar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Balsarkar GD. Role of peripartum cesarean section in maternal collapse in pregnancy. Wadia J Women Child Health. 2024;3(1):31-4. doi: 10.25259/WJWCH_11_2022
Abstract
Fortunately, maternal cardiopulmonary arrest is an uncommon complication in the field of obstetrics, nevertheless dreaded by the clinicians. Perimortem cesarean section (PMCS), if performed in a timely manner, not only improves the chances of fetal survival but also improves the success rates of maternal resuscitation. In pregnant women over 20 weeks of gestation, if there is no response to correctly performed cardiopulmonary resuscitation within 4 min of maternal collapse or if resuscitation is required to be continued beyond this time, then perimortem cesarean section should be undertaken to assist maternal resuscitation. Delivery of the fetus and placenta reduces oxygen consumption and improves venous return and cardiac output, facilitates chest compressions, and makes ventilation easier. PMCS should be considered a resuscitative procedure, to be performed primarily in the interests of maternal survival. Delivery within 5 min of maternal collapse improves the chances of survival for the baby. A case of maternal collapse due to cardiac tamponade with aortic dissection where a live baby was delivered by perimortem cesarean section is described.
Keywords
Post-mortem
Perimortem
Cesarean delivery
Cardiopulmonary arrest
INTRODUCTION
Fortunately, maternal cardiopulmonary arrest is an uncommon complication in the field of obstetrics but that also makes an obstetrician nervous and underprepared when this dreaded complication happens. Perimortem cesarean section (PMCS), if performed in a timely manner, not only improves the chances of fetal survival but also the success rate of maternal resuscitation. In women over 20 weeks of gestation, if there is no response to correctly performed cardiopulmonary resuscitation (CPR) within 4 min of maternal collapse or if resuscitation is continued beyond this, then perimortem cesarean section should be undertaken to assist maternal resuscitation. This case report is of a PMCS performed within a short time of maternal collapse with a good fetal outcome.
CASE REPORT
A 30-year-old previously healthy patient, second gravida with one previous abortion presented at 40-week gestation with complaints of sudden onset of sharp, shooting chest pain, radiating to back associated with dyspnea. She had no other known medical or surgical illnesses. On examination, her pulse rate was 70 beats/min, feeble, and systolic blood pressure (BP) of 90 mmHg and diastolic was not recordable. She was conscious and oriented, afebrile with no pallor, cyanosis, or icterus. On per abdominal examination, uterus was full term, with cephalic presentation. Fetal heart rate was 144 beats/min. The patient was immediately shifted to emergency medicine services, where she was infused with crystalloids and her diastolic BP became recordable. Cardiac examination and electrocardiogram were unremarkable. She was admitted to the medicine ward and was treated symptomatically for suspected gastroesophageal reflux. Two days later, she was referred to the obstetrics department. Labor was induced with dinoprostone gel in view of postdatism. After 6 h of labor induction, the patient suddenly became cyanosed and vitals were not recordable. Cardiopulmonary resuscitation (CPR) was initiated and the patient was intubated. To improve resuscitative measures, within 4 min, an emergency perimortem cesarean delivery was performed using pfannenstiel incision and lower uterine segment transverse incision and a baby boy was delivered and transferred to the Neonatal Intensive Care Unit. Meanwhile, CPR continued but the mother could not be revived at the end of 2 h. Post-mortem analysis revealed a diagnosis of cardiac failure due to cardiac tamponade secondary to aortic dissection [Figures 1 and 2].
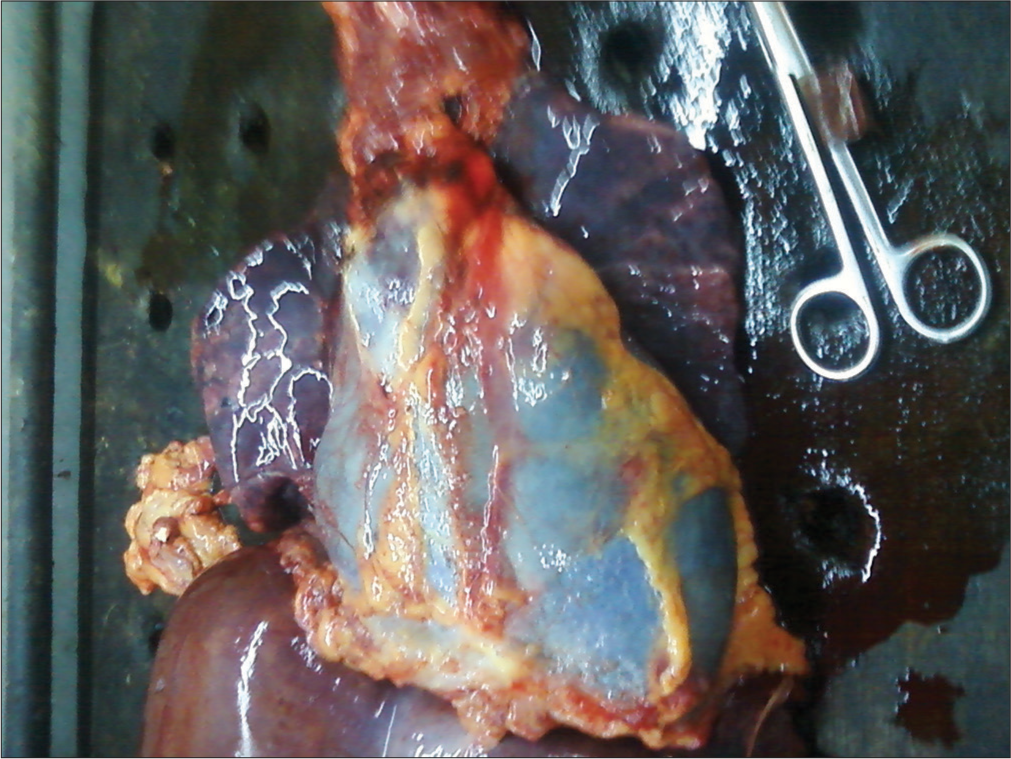
- Cardiac tamponade on post-mortem of sudden maternal collapse.
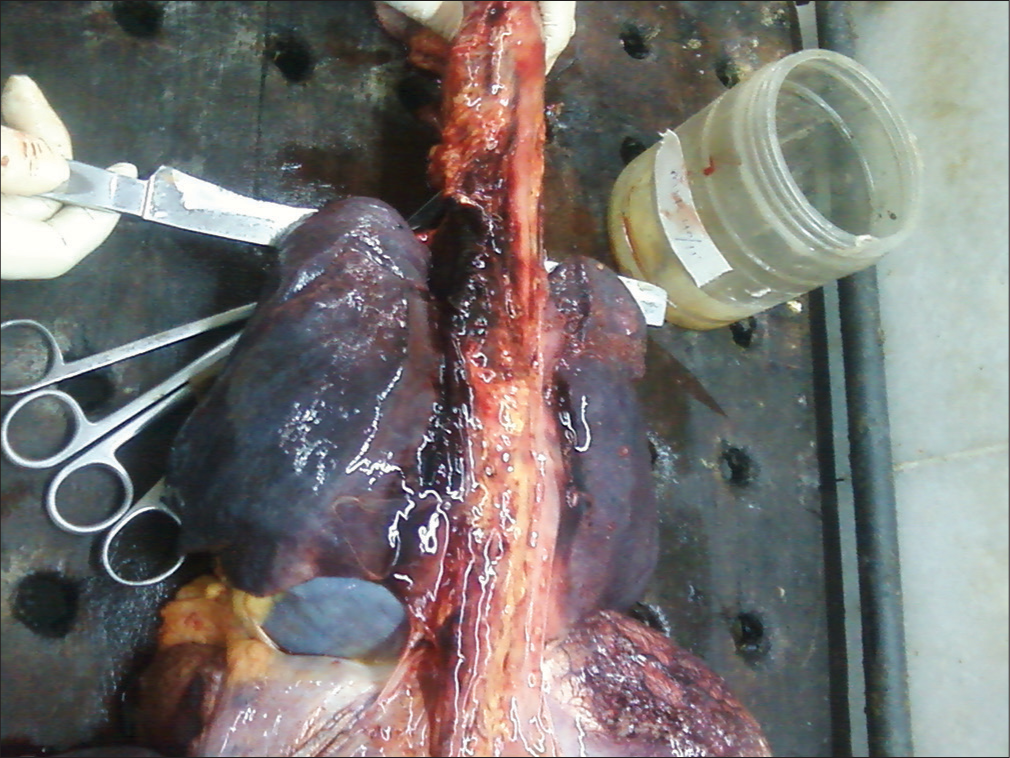
- Aortic dissection on post-mortem of sudden maternal collapse.
DISCUSSION
Maternal collapse can result from a number of causes. A systematic approach should be taken to identify the cause. Aortocaval compression significantly reduces cardiac output from 20 weeks of gestation onwards and reduces the efficacy of chest compressions during resuscitation. Changes in lung function, diaphragmatic splinting, and increased oxygen consumption make pregnant women hypoxic more readily and make ventilation more difficult. Pregnant women are at an increased risk of aspiration.[1]
Manual displacement of the uterus to the left is effective in relieving aortocaval compression in women above 20 weeks’ gestation or where the uterus is palpable at or above the level of the umbilicus. This permits effective chest compressions in the supine position in the event of cardiac arrest. A left lateral tilt of the woman from head to toe at an angle of 15– 30° on a firm surface will relieve aortocaval compression in the majority of pregnant women and still allow effective chest compressions to be performed in the event of cardiac arrest.
Intubation in an unconscious woman with a cuffed endotracheal tube should be performed immediately by an experienced intensivist or anesthetist. Supplemental high-flow oxygen should be administered as soon as possible to counteract rapid deoxygenation.[2] If the airway is clear and there is no breathing, chest compressions and ventilation should be commenced immediately.[3]
In women over 20 weeks of gestation, if there is no response to correctly performed CPR within 4 min of maternal collapse or if resuscitation is continued beyond this period of time then perimortem cesarean section should be undertaken to assist maternal resuscitation. Ideally, this should be achieved within 5 min of the collapse. PMCS should not be delayed by moving the woman to another place but rather should be performed where maternal collapse has occurred and resuscitation is taking place. The operator should use an incision which will facilitate the most rapid access. This may be a midline vertical incision or a suprapubic transverse incision. A scalpel and umbilical cord clamps (or alternative ligatures) should be available on the resuscitation trolley in all areas of the hospital where pregnancy care is provided and maternal collapse may occur, including the accident and emergency department.[4]
From around 20 weeks of gestation and beyond, the gravid uterus reduces venous return in the supine position. As a consequence, cardiac output is reduced by up to 30–40%. Supine hypotension itself can precipitate maternal collapse, which is usually reversed by turning the woman into the left lateral position. When cardiopulmonary arrest occurs, chest compressions are needed to produce a cardiac output. In the non-pregnant situation, this is expected to achieve around 30% of the normal cardiac output. Aortocaval compression further reduces cardiac output to approximately 10% of the non-pregnant cardiac output. Therefore, CPR is less likely to be effective in a woman who is at 20 or more weeks of gestation.[5]
Changes in lung function, diaphragmatic splinting, and increased oxygen consumption make pregnant women become hypoxic more readily and make ventilation more difficult. The increased progesterone level in pregnancy increases the respiratory drive, leading to an increase in tidal volume and minute ventilation. Splinting of the diaphragm by the enlarged uterus reduces the functional residual capacity (FRC) and also makes ventilation more difficult. Reduction in FRC, along with the markedly increased oxygen consumption of the fetoplacental unit means that pregnant women become hypoxic much more rapidly during periods of hypoventilation.[6]
The concept of perimortem cesarean section was introduced by Katz et al. 80 in 1986.[5] This research group initially focused on infant survival and found that 69% of infants survived when PMCS was performed within 5 min. However, when Katz et al.[5] explored maternal outcomes, they found that hypoxic brain injury only occurred if PMCS was performed after 6 min. The term “resuscitative hysterotomy” has been used for this procedure. The gravid uterus impairs venous return and thus reduces cardiac output by approximately 60% secondary to aortocaval compression. Delivery of the fetus and placenta reduces oxygen consumption, improves venous return and cardiac output, facilitates chest compressions, and makes ventilation easier. It also allows for internal/direct chest compressions by inserting the hand through the open abdomen up to the diaphragm and compressing the posterior aspect of the heart against the chest wall. This improves cardiac output beyond that achieved in closed chest compressions. At less than <20 weeks of gestation, there is no proven benefit from delivery of the fetus and placenta. PMCS should be considered a resuscitative procedure, to be performed primarily in the interests of maternal survival.[7]
Delivery within 5 min of maternal collapse improves the chances of survival of the baby. If maternal resuscitation continues beyond 4 min of the collapse, delivery of the fetus and placenta should be performed as soon as possible to aid this, even if the fetus is already dead. Case series have shown that swift delivery of the baby improves maternal outcome even after 5 min have elapsed from maternal collapse.
Time should not be wasted by moving the woman to an operating theatre; a PMCS can be performed anywhere, with a scalpel being the only essential equipment required. With no circulation, blood loss is minimal, and no anesthetic is required. If resuscitation is successful following birth, there should be prompt transfer to an appropriate environment at that point, as well as anesthesia and sedation, to control the ensuing hemorrhage and complete the operation. The doctrine of “best interests of the patient” would apply to the conduct of this procedure being carried out without consent.
In terms of the best incision to use, a midline abdominal incision and a classical uterine incision will give the most rapid access. If resuscitation is successful, the uterus and abdomen should be closed in the usual way to control blood loss and minimize the risk of infection.
To ensure there are no delays in executing a PMCS when indicated, the equipment necessary should be immediately available on the resuscitation trolley. All that is required is a fixed-blade scalpel and two clamps for the umbilical cord. In the absence of a specific tray, a scalpel alone will enable the delivery of the fetus and placenta.
The systematic review to study the efficacy of PMCS was published by Einav et al. identified a total of 80 relevant publications that reported the outcome of 94 women. In 31.7% of identified cases of PMCS, the procedure was found to be of benefit for maternal or fetal survival. No harm was found in any of the 94 women who underwent PMCS. When analyzing maternal outcomes, 54.3% of women survived until hospital discharge and 42.6% of women survived with good-to-moderately impaired neurological outcomes. Although the study was unable to validate the need to deliver by 5 min duration, it was able to demonstrate that maternal outcomes were more favorable if performed within 10 min of maternal cardiac arrest (OR 7.42; P < 0.05). Neonatal survival was also associated with a shorter mean cardiac arrest to delivery time. Neonatal survival was found only in women who suffered cardiac arrest in hospital and there are reports of neonatal survival when delivery was performed by 30 min of maternal cardiac arrest.[7]
CONCLUSION
Perimortum caesarean section should be performed in critical patients immediately to save the baby and help in resuscitation of the mother.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- RCOG green-top guideline no. 56 e32 of e52 ª Royal College of obstetricians and gynaecologists.
- [Google Scholar]
- Management of cardiac arrest in pregnancy: A systematic review. Resuscitation. 2011;82:801-9.
- [CrossRef] [PubMed] [Google Scholar]
- Challenging the 4-to 5-minute rule: From perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2016;215:129-31.
- [CrossRef] [PubMed] [Google Scholar]
- Perimortem caesarean section-why, when and how. Obstet Gynaecol. 2018;20:151.
- [CrossRef] [Google Scholar]
- Perimortem caesarean delivery: Were our assumptions correct? Am J Obstet Gynecol. 2005;192:1916-21.
- [CrossRef] [PubMed] [Google Scholar]
- Perimortem cesarean section for maternal and fetal salvage: Concise review and protocol. Acta Obstet Gynecol Scand. 2014;93:965-72.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal cardiac arrest and perimortem caesarean delivery: Evidence or expert-based? Resuscitation. 2012;83:1191-2000.
- [CrossRef] [PubMed] [Google Scholar]






