Translate this page into:
Osteoarticular tuberculosis in infants: A diagnostic and management challenge
-
Received: ,
Accepted: ,
How to cite this article: Shah S, Nathani P, Aroojis A, Agashe MV, Mehta R. Osteoarticular tuberculosis in infants: A diagnostic and management challenge. Wadia J Women Child Health. 2023;2(3):104-7. doi:10.25259/WJWCH_33_2023
Abstract
Objectives:
Musculoskeletal manifestations of tuberculosis in infants are rare and different both in etiopathological mechanism and clinical presentation. Radiological diagnosis of osteoarticular tuberculosis (TB) in infants is tricky due to the various differentials of a cystic lesion. Literature also mention it only in isolated case reports. We carried out this study with an aim to collate and study patterns of osteoarticlular TB in the appendicular skeleton and to highlight the difficulties in diagnosis and management.
Material and Methods:
We retrospectively reviewed the data at our hospital over the past 8 years. Microbiologically confirmed osteoarticular tuberculosis affecting appendicular skeleton in children below 1 year of age were included in the study. Cases with spine involvement were excluded. The delay to diagnosis from the onset of symptoms, the initial diagnosis and treatment given were noted. The resolution of radiological presentation and occurrence of deformities at the final follow up (atleast 1 year) were noted.
Results:
During the study period, 8 infants were diagnosed to have osteoarticular tuberculosis with median age at presentation of 8.7 months (range 3 to 12 months). Average duration of follow up was 4 years (range 1 to 8 years). Cystic, Erosive, infiltrative, spina ventosa and mortar pestle were the radiological appearances found. Three of the 8 cases were referred as suspected malignancy. All but one case were vaccinated with BCG. Curettage and anti-tubercular therapy (ATT) were the treatment in all cases. Three cases with a delay in diagnosis of more than 2 months, developed complications: 1 had limb length discrepancy (LLD) due to physeal involvement, 1 developed angular deformity and 1 child had perthe’s disease as a sequelae.
Conclusion:
Osteoarticular tuberculosis is an increasing possibility, shockingly, even in infancy and should be a differential in an endemic country like India. A delay to diagnosis of even 2 months of this condition can lead to devastating complications. Being mindful of the diagnosis and early treatment gives rewarding results.
Keywords
Infant
Tuberculosis
Osteomyelitis
Infection
INTRODUCTION
Tuberculosis (TB) is endemic in India and childhood tuberculosis accounts for a third of children with TB globally. Its incidence has been increasing in recent years in the Western world. Literature rates the incidence of osteoarticular TB to be roughly 11–15% of all cases of extrapulmonary TB.[1] However, in the pediatric population, they consist of only about 5–6% of all extrapulmonary cases.[2] Spinal TB accounts for approximately half of all cases of musculoskeletal TB.[3]
The pediatric age group has different pathophysiological mechanism of TB infection. In infants, a primary complex, similar to bacterial infections, is the likely cause compared to older children and adults where reactivation and/or spread of bacilli from a primary pulmonary focus is the cause.[4] The characteristics of tuberculous osteomyelitis in children are also different from those in adults making them a challenge to diagnose for the clinician. The clinical findings are not specific and are even more difficult to elicit in infants. It has a variety of close radiological mimics which cause a delay in the diagnosis and treatment, ultimately affecting the growth of the pediatric bone. These variegated presentations require a timely diagnosis to prevent the debilitating sequelae. Surgery and anti-tubercular therapy (ATT) remain the mainstay in the management of these cases. We undertook this study to understand the presentation and outcome in infants diagnosed with osteoarticular TB.
MATERIAL AND METHODS
This was a retrospective study carried out at a tertiary referral center in western India over a period of 8 years. Data for the study were obtained from medical records maintained in the indoor and outpatient sections. Parental consent was obtained for this study.
All children less than one year of age, presenting between 2014 and 2022 with microbiologically confirmed diagnosis of Mycobacterium tuberculosis infection of the osteoarticular system with a minimum of one year follow up were included. Children with involvement of spine were excluded from the study. During the study period, eight infants matched the inclusion criteria. Data collected included the age of the child at diagnosis, duration of symptoms at presentation, gender, the bone involved, type of lesion (radiological), laboratory data including microbiological finding, presence of dissemination, and advanced imaging were noted.
Details of surgical procedures and adjuvant treatments, clinical and radiological healing progress, and outcome observed during the last follow-up, as well as any complications, including instances of local recurrence were recorded.
RESULTS
Eight children were diagnosed with osteoarticular TB during the study period. There were 6 boys and 2 girls with the median age at presentation of 8.7 months (range 3 to 12 months). The duration of the symptoms ranged from 2 weeks to 3 months. The average duration of follow-up was 4.2 years (range 12 months to 8 years). The lesions were localized in the proximal tibia in three children and metaphyseal radius, phalanx, distal femur metaphysis, hip, and ankle joint in one child each. The radiological type was varied [Figure 1].

- Four different cases of infantile tuberculosis with varied sites and radiological affection.
Only two of the eight children were referred with possible suspicion of an underlying infection. The primary presenting diagnoses were – tumor, nutritional deficiency and congenital deformity. The average delay to diagnosis was 48 days (range, 15 to 90 days). All of these lesions were confirmed to be TB by microbiology. Curettage followed by ATT according to the existing Revised National Tuberculosis Control Programme protocol was provided to all according to their weight. One of the children with proximal tibia involvement had rifampicin resistance and was given treatment as per the multidrug-resistant TB protocol. Seven of them went on to heal radiologically without recurrence at the final follow-up.
Complications were seen in three children. One child with hip joint involvement developed Perthes-type sequelae. Two children with proximal tibial involvement developed an affection of the physes, of which one developed limb length discrepancy (LLD) of 1.5 cm at 4 years of follow up [Figure 2] and the other one developed an angular deformity that was slowly progressing. Notably, all three children with complications had presented to us late, after 2 months of onset of symptom.
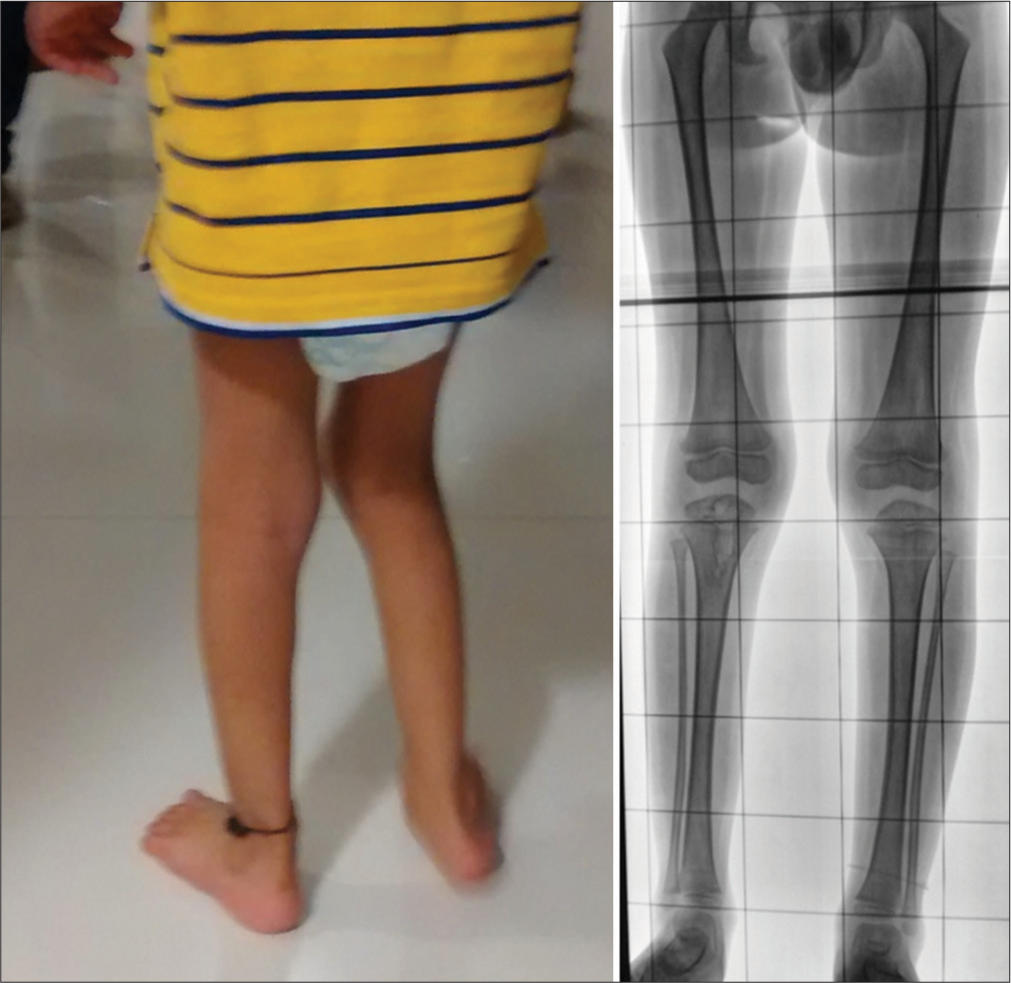
- A child at follow-up of 4 years has a limb length discrepancy of 1.5 cm.
DISCUSSION
Bone and joint involvement in TB is uncommon. Pediatric presentation of osteoarticular TB is even rarer. Recent literature in western India quotes 8% of extrapulmonary TB cases to be osteoarticular.[5] Literature is scarce on osteoarticular TB in infants. After an exhaustive search on PubMed, we found two isolated case reports that mentioned osteoarticular TB in infants.[6,7] Here, we present a series of eight different cases of osteoarticular TB presenting in infancy, their presentation, and treatment.
Agrawal and Khan mentioned that in young children and infants, the lesion of TB usually occurs as a primary complex without any underlying primary infection of the lung or the abdomen.[8] This is in contrast to older children and adults where skeletal TB usually is secondary to primary pulmonary or abdominal TB. Another etiology that has been presented is horizontal spread from an infected mother or close relatives to the child.[9] Most of the TB cases were seen in unvaccinated children. In our series, none of the children had a pulmonary involvement on a chest radiograph. All but one child had been vaccinated for TB.
Being a cold abscess, tuberculous osteomyelitis presents with non-specific clinical findings in a child. Examination of an irritable child with pain is also difficult. Localized pain, and limp (in lower limb involvement) have been mentioned as the clinical findings in a child with TB. The symptoms at the presentation in our series were also vague as also in other studies.[10,11] Due to early presentation in an infant and relatively short history, constitutional symptoms were absent. Pain and swelling were consistent finding in all cases. Limp was evident in five cases where lower limbs were involved.
Erythrocyte sedimentation rate (ESR) elevation has been shown in various studies to be a good marker for the prediction of bone TB.[5,12] In our study, all cases had significant elevation of ESR.
Radiographs have been the mainstay for the diagnosis of TB. Rasool has categorized tuberculous lesions into four basic types: (a) Cystic; (b) infiltrative; (c) focal erosions; and (d) spina ventosa.[13] In our series, we were able to see all of these types which were described. The type of lesion did not change the management which in all cases was debridement, curettage, biopsy and ATT.
CONCLUSION
Osteoarticular TB is an increasing possibility, even in infancy. A delay to diagnosis of even 2 months of this condition can lead to devastating complications. Being mindful of the diagnosis and early treatment gives rewarding results.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Navicular tuberculosis: A rare localization of bone tuberculosis. IDCases. 2015;2:80-2.
- [CrossRef] [PubMed] [Google Scholar]
- General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:11-9.
- [CrossRef] [PubMed] [Google Scholar]
- Spinal tuberculosis: A review. J Spin Cord Med. 2011;34:440-54.
- [CrossRef] [PubMed] [Google Scholar]
- Paediatric osteoarticular tuberculosis: A review. J Clin Orthop Trauma. 2020;11:202-7.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of osteoarticular tuberculosis in children. Indian J Tuberc. 2020;67:43-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tuberculosis of distal radius presenting as a cystic lesion in a nine-month-old infant: A rare case report. J Clin Diagn Res JCDR. 2016;10:RD06.
- [CrossRef] [PubMed] [Google Scholar]
- Sternal tuberculosis in a 9-month-old infant after BCG vaccination. Acta Paediatr. 2000;89:1495-7.
- [CrossRef] [PubMed] [Google Scholar]
- Multifocal osteoarticular tuberculosis in children. J Ortho Surg (Hong Kong). 2011;19:336-40.
- [CrossRef] [PubMed] [Google Scholar]
- Management of newborn infant born to mother suffering from tuberculosis: Current recommendations and gaps in knowledge. Indian J Med Res. 2014;140:32-9.
- [Google Scholar]
- Bone and joint tuberculosis: A review of 652 cases. Orthopedics. 1988;11:861-6.
- [CrossRef] [PubMed] [Google Scholar]
- Erythrocyte sedimentation rate in childhood tuberculosis: Is it still worthwhile? Int J Tuberc Lung Dis. 2000;4:237-9.
- [Google Scholar]
- Tuberculosis-the masquerader of bone lesions in children. SA Orthop J. 2009;8:21-5.
- [Google Scholar]







