Translate this page into:
Transabdominal cerclage: The journey of turning bad into good
*Corresponding author: Sweta Shrivastava, Department of Obstetrics and Gynaecology, Nowrosjee Wadia Maternity Hospital, Mumbai, Maharashtra, India. swetashrivastava24@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pawar A, Shrivastava S, Kadrekar A. Transabdominal cerclage: The journey of turning bad into good. Wadia J Women Child Health 2023;2(2):100-3.
Abstract
Recurrent pregnancy loss is a challenging obstetric condition that requires thorough evaluation and vigilant antenatal care. Cervical insufficiency is a well-recognized cause of late miscarriage. Here, we are reporting a case of multiple pregnancy failures including both 1st- and 2nd-trimester losses with cervical insufficiency after ruling out all other probable causes. The patient had a history of 3 failed transvaginal cervical cerclage procedures, and hence, in her 7th pregnancy, transabdominal cervical cerclage was attempted that resulted in salvaging the pregnancy beyond viability and the patient delivered a healthy baby through an emergency cesarean section near term. The patient was reconceived with the transabdominal cerclage in situ and delivered with a successful fetal and maternal outcome despite having multiple high-risk factors. This highlights the effectiveness of transabdominal cervical cerclage to prevent spontaneous mid-trimester loss and preterm delivery when previous transvaginal cerclage has failed.
Keywords
Recurrent pregnancy loss
Transabdominal cerclage
Vaginal cerclage
Cervical insufficiency
INTRODUCTION
As per the Royal College of Obstetricians and Gynaecologists (RCOG), recurrent pregnancy loss (RPL) is defined as the loss of three or more consecutive pregnancies. The loss of a baby either in utero or after birth is always a devastating experience for a mother. Multiple pregnancy failure is a challenging situation for the couple as well as for the obstetrician. Cervical insufficiency is a clinical diagnosis based on the history of a spontaneous mid-trimester loss associated with painless cervical dilation in the absence of other causes (e.g., labor, trauma, major fetal anomaly, stillbirth, etc.). The incidence of cervical insufficiency in the general obstetric population is between 1/100 and 1/2000 live births.[1] The mainstay of cervical insufficiency treatment is cerclage, which may be placed through the vaginal route or placed higher (cervico-isthmic) through abdominal route. The transabdominal cerclage (TAC) procedure is reserved for women who have previously failed transvaginal cerclage.
CASE REPORT
A 30-year-old woman, 7th gravida with previous six abortions got registered at our institute at 7 weeks 3 days of gestation. All conceptions were spontaneous, of which three were 1st-trimester abortions and three were 2nd-trimester abortions (16 and 19 weeks). She had a history of cervical cerclage done vaginally in all three 2nd trimester abortions. Considering her previous three failed cerclage procedures the patient was posted for open abdominal cervical cerclage at 10 weeks of gestation. The intraoperative and post-operative period was uneventful. Anti D 50 mcg intramuscular injection was given post-procedure as she had rhesus (Rh)-negative blood group status. The patient remained admitted in the hospital for monitoring and assessment purposes.
The patient was on progesterone support and folic acid supplementation. Her pregestational hypothyroidism was well controlled with thyroxine replacement therapy.
At 22 weeks, the patient complained of threatened preterm labor so oral tocolytic therapy was initiated. The patient developed gestational diabetes mellitus (GDM) and early-onset pre-eclampsia between 24 and 26 weeks which were effectively controlled with insulin and oral antihypertensive drugs.
At 34 weeks, tocolysis was stopped and at 34 weeks 5 days, she went into spontaneous labor. An emergency lower segment cesarean section (LSCS) was done because of the bad obstetric history with abdominal cerclage and gestational hypertension (HTN), gestational diabetes mellitus, hypothyroidism and Rh-negative status. The transabdominal cervical cerclage knot was left in situ. The patient delivered a live male baby with 2.5 kg birth weight, who cried immediately after birth, and was shifted to the neonatal intensive care unit for monitoring. Mother and baby were discharged on the 5th-day post-LSCS.
Subsequently in the 7 years with the cervical cerclage in situ, the patient had three more conceptions, of which the initial two resulted in 1st-trimester failures and she got registered at our institute as a 10th gravida. From the start, this pregnancy was supported with folic acid, aspirin, and progesterone support. This 10th pregnancy was associated with pregestational hypothyroidism and gestational HTN, but blood sugar levels were well controlled throughout the pregnancy.
At 35 weeks 5 days, she reported in the emergency in early labor and an emergency cesarean section was done. A live male baby of 2.6 kg birth weight was delivered. The mother and baby had an uneventful postnatal period and were discharged on day 4.
DISCUSSION
The risk of miscarriage increases after each successive pregnancy loss and is approximately 40% after three consecutive losses. The prevalence of RPL is about 1–3%.[2] International evidence-based guidelines for the management of RPL have been published in recent years by the RCOG in 2011, the American Society for Reproductive Medicine in 2012, and the European Society of Human Reproduction and Embryology in 2017. It is important to establish the cause to prevent further losses. Cervical incompetence is the most common cause of recurrent 2nd-trimester loss. The mainstay of cervical insufficiency treatment is cerclage, which may be placed vaginally or abdominally. Failure of prophylactic transvaginal cerclage in women with cervical insufficiency justifies the need for a TAC. There are no clear guidelines regarding the indication of TAC, and it is usually performed in patients who cannot undergo the transvaginal approach as in case of traumatic laceration, congenital or surgical shortening of the cervix, scarred cervix, or having previously failed transvaginal cerclage.[3]
The TAC is placed at the cervico-isthmic portion of the uterus, while transvaginal cerclage often ends up distal to the internal os. Thus, in cases of scarred cervix or amputated cervix where the placement of cerclage is not possible vaginally, the transabdominal approach allows higher placement of cerclage [Figure 1].
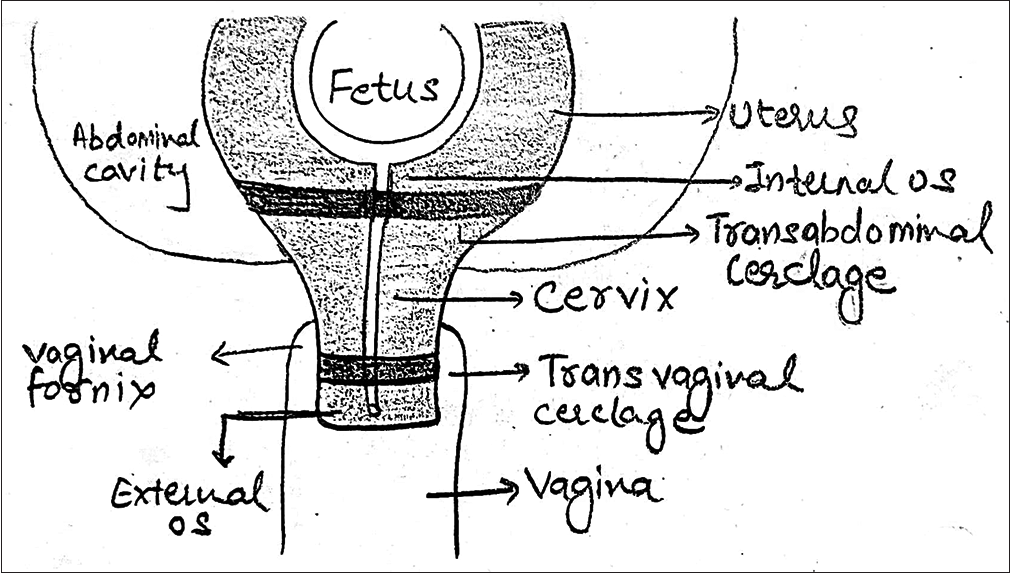
- Schematic representation of placement of transabdominal and tranvaginal cerclage.
The trans-abdominal cervico-isthmic cerclage results in better birth outcomes than the transvaginal approach.
TAC can be performed before or during the early weeks of pregnancy either laparoscopically or by laparotomy.
TAC was first described by Benson and Durfee in 1965. One of the most important steps of TAC is to identify avascular space between uterine vessels and the uterus and to place the cerclage stitch correctly in this avascular area.
In cases of cerclage done before pregnancy, the cerclage thread can act as a foreign body and can be a cause of intra-abdominal foreign body reaction. On the other hand, if we perform TAC early in the pregnancy, there is a risk of abortion. The procedure itself can be a cause of uterine contractions.
During pregnancy uterine vessels are usually expanded to support fetal growth, there is a risk of damage to these vessels during the procedure, which can be a cause of massive bleeding and abortion.
In a retrospective cohort study including 300 TACs performed over a period of 24-years 11 (3.7%) surgical complications were encountered. Fetal loss (before 20 weeks) occurred in 4.1% of pregnancies. The median estimated blood loss was 100 mL, with blood loss requiring transfusion only once. Lower uterine dehiscence in four patients and uterine rupture in one suggest the advisability of early-term delivery after fetal lung maturity is assured. Results of the study demonstrate that complications encountered in placing a TAC were unusual and generally manageable.[3,4]
The greatest disadvantage of TAC through laparotomy is that it requires at least two extra laparotomies (cerclage and removal). With this procedure, a safe vaginal birth is impossible, and cesarean section is required.
To prevent multiple laparotomies, a laparoscopic procedure or a robot-assisted procedure can be an alternative. Laparoscopic procedures seem to be more complicated, take more time and need expertise to perform the procedure.
A cohort study conducted for 96 pregnancies who underwent TAC before or during pregnancy resulted in a 93% success rate.[5]
A retrospective and prospective cohort study conducted over 22 years reported that pre-conceptional TAC as compared to first-trimester TAC is more successful in preventing repeat spontaneous mid-trimester loss and preterm labor and is associated with less surgical and pregnancy-related morbidity.[6]
A meta-analysis report concludes that the laparoscopic and open laparotomy abdominal cerclage placements at intervals or during pregnancy, produced similar outcomes in terms of survival and gestational age at the time of delivery. There were some differences in perioperative care, surgical complications, interventions required, and complications during pregnancy. This implies that both methods of abdominal cerclage placement have high success rates.[7]
As for sutures for TAC, non-absorbable thick braided synthetic polyester fiber sutures, such as Mersilene™ or Teflon™ with a 3–5 mm width, are used in many institutes. Some institutes prefer to use thinner monofilament threads such as nylon thread for the cerclage. Thick braided synthetic polyester fiber sutures have higher tensile strength than thinner monofilament threads. In our case, mersilene tape was used and the knot was placed posteriorly.
When abortion is detected with an abdominal cerclage knot in situ, it is usually possible to dilate the cervical canal up to the size of a number 5 Hegar dilator. With this size of dilatation, it is possible to insert a suction tube for removing the embryo in the first trimester.
Regarding progesterone support during pregnancy, National Institute of Clinical Excellence (NICE), in the United Kingdom, International Federation of Gynecology and Obstetrics FIGO, and the Society for Maternal-Fetal Medicine (SMFM), United States all recommend the use of progestogens in women at high risk of preterm birth. SMFM advises the use of 17-hydroxyprogesterone caproate (250 mg intramuscularly weekly) starting at 16–20 weeks until 36 weeks or delivery for women with a singleton gestation and a history of prior spontaneous preterm birth. The two former organizations endorse the use of vaginal progesterone for women with a short cervix.[8]
CONCLUSION
Every pregnancy needs proper antenatal care and individual assessment. In such a case, where pregnancy is deemed precious, achieved after recurrent losses and then complicated with multiple risk factors throughout the course, it is extremely challenging for the obstetrician to manage the patient clinically and psychologically. Transabdominal cerclage (TAC) is an option to provide better outcomes in such women with RPL. TAC requires vigilant monitoring and periodic evaluation to improve outcomes.
Proper counseling, reassurance, psychological support, institutional care, and timely interventions have made it possible to turn a bad obstetric history into a good fetal outcome.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Current management of recurrent pregnancy loss. Obstet Gynaecol. 2022;24:260-71.
- [CrossRef] [Google Scholar]
- Transabdominal cerclage (TAC) as a new tool for the treatment of cervical incompetence (CI) Ann Transl Med. 2020;8:571.
- [CrossRef] [PubMed] [Google Scholar]
- Operative complications and fetal morbidity encountered in 300 prophylactic transabdominal cervical cerclage procedures by one obstetric surgeon. J Obstet Gynaecol. 2011;31:713-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transabdominal cerclage: Can we predict who fails? J Matern Fetal Neonatal Med. 2007;20:63-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transabdominal cerclage: Preconceptual versus first trimester insertion. Eur J Obstet Gynecol Reprod Biol. 2016;199:27-31.
- [CrossRef] [PubMed] [Google Scholar]
- The effectiveness of transabdominal cerclage placement via laparoscopy or laparotomy: A systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2023;5:100757.
- [CrossRef] [PubMed] [Google Scholar]
- Progesterone and preterm birth. Int J Gynecol Obstet. 2020;150:24-50.
- [CrossRef] [PubMed] [Google Scholar]






