Translate this page into:
Neuropsychiatric lupus: An uncommon presentation of pediatric systemic lupus erythematosus
*Corresponding author: Abhismita Priyadarshinee, Department of Pediatrics, B J Wadia Hospital for Children, Mumbai, Maharashtra, India. abhismitapriyadarshinee@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Priyadarshinee A, Kini S, Ohri A. Neuropsychiatric lupus: An uncommon presentation of pediatric systemic lupus erythematosus. Wadia J Women Child Health. 2024;3:93-8. doi: 10.25259/WJWCH_29_2024
Abstract
Systemic lupus erythematosus (SLE) is a multisystemic autoimmune disease with a variety of clinical manifestations and several immune-mediated abnormalities leading to multiple organ dysfunction. In adult-onset SLE, neurological symptoms and polyarthritis predominate, whereas in children and adolescents, lupus nephritis, hematological disorders, photosensitivity, butterfly rash, and mucosal ulceration are more common. We describe the case of a 16-year-old boy presenting with fever, rash, seizures, ultimately diagnosed with neuropsychiatric lupus. Laboratory findings, including positive autoantibodies and neuroimaging suggestive of central nervous system involvement, supported the diagnosis. Treatment comprised steroids, cyclophosphamide, and adjunctive therapy, leading to clinical amelioration. Neuropsychiatric SLE management focuses on symptomatic relief and halting underlying disease processes, often requiring immunosuppressive therapy. This case underscores the varied clinical spectrum of childhood SLE and highlights the pivotal role of steroids and cyclophosphamide in managing neuropsychiatric manifestations.
Keywords
Systemic lupus erythematosus
Neuropsychiatric lupus
Seizure
Immunosuppressive therapy
INTRODUCTION
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease characterized by a fluctuating course and a wide array of clinical manifestations. Neuropsychiatric involvement in SLE encompasses a spectrum of neurological and psychiatric symptoms that impact both the central and peripheral nervous systems. Approximately 25% of children with SLE have neuropsychiatric manifestations of SLE which significantly contribute to morbidity and mortality.[1] The variability in clinical presentation and the extensive differential diagnoses pose significant challenges to accurate diagnosis and treatment. A heightened clinical suspicion, in conjunction with laboratory and neuroimaging findings, is essential for confirming the diagnosis. This case report discusses a 16-year-old male who presented with fever, rash, and seizures, diagnosed with neuropsychiatric lupus and treatment with corticosteroids and cyclophosphamide resulted in significant clinical improvement.
CASE REPORT
A 16-year-old boy presented with a low-grade, intermittent fever since 1 year, associated with maculopapular rash over the face, both arms, and palatal ulceration for 1 week and two episodes of generalized tonic-clonic seizures lasting 4-5 minutes and subsiding spontaneously. In addition, there was a history of a 10 kg weight loss over 5 months.
On examination, the child had pallor, palatal ulcer, maculopapular rash across the face and bilateral arms, along with hyperpigmented rash evident on the trunk [Figures 1-3]. The child was normotensive, and without signs of meningeal irritation.

- Palatal ulcer.

- Macular rash over face.
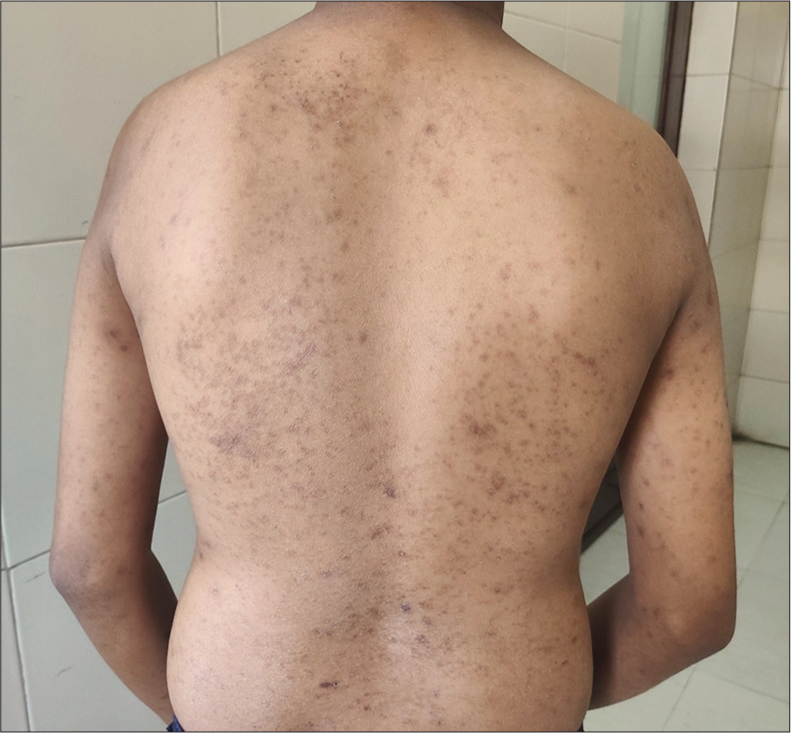
- Macular rash over back.
Autoimmune conditions, particularly systemic lupus erythematosus (SLE) was considered. Baseline blood investigations revealed hemoglobin of 8.7 mg/dl, total leucocyte count (TLC) of 4,600c/mm3, platelet count of 3.34 lakh, C-reactive protein 1, and erythrocyte sedimentation rate of 49 [Table 1].
| ANA | 1:320 | |
| ANA Blot | ||
| Anti ds DNA antibody | Positive | |
| Anti Ribosome PO antibody | Strong positive | |
| Anti Histone antibody | Positive | |
| Anti Nucleosome antibody | Positive | |
| Anti Mi-2β antibody | Positive | |
| Anti AMA M2 antibody | Positive | |
| C3 | 51 (90-180) | |
| C4 | 2.21 (12-43) | |
| DCT | Weakly positive (0.5) | |
| Antiphospholipid antibody domain | Anti Cardiolipin antibody | Weak positive |
| Anti B2 Glycoprotein antibody | Negative | |
| Lupus Anticoagulant antibody | Negative |
ANA: antinuclear antibody, ds DNA: double stranded Deoxyribonucleic acid, PO: Protein, Anti AMA M2: anti mitochondrial M2, DCT: Direct Coombs test
Magnetic Resonance Imaging (MRI) brain revealed acute left insular cortex bleed with significant surrounding edema, acute non-hemorrhagic infarct along the left posterior watershed area, and multiple white matter hyperintense lesions in bilateral parietal region – suggestive of central nervous system (CNS) involvement in SLE [Figures 4-6].
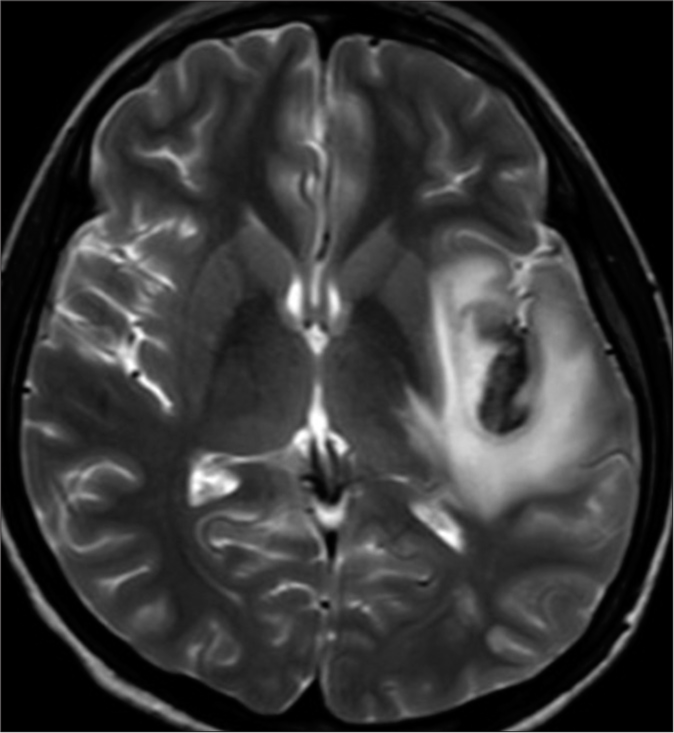
- Axial T2-weighted hyperintense lesion with a central dark area in the left insular cortex with perilesional edema.
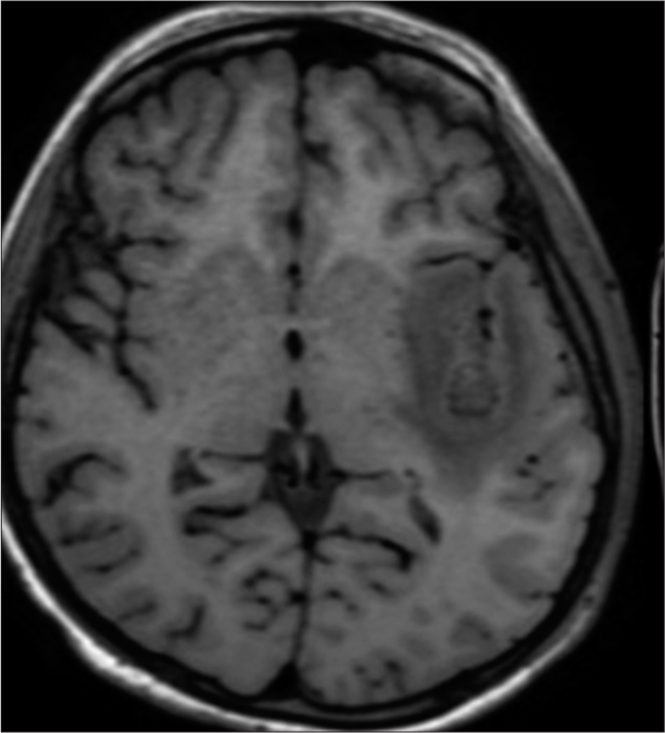
- Axial T1-weighted hypointense lesion in the left insular cortex.
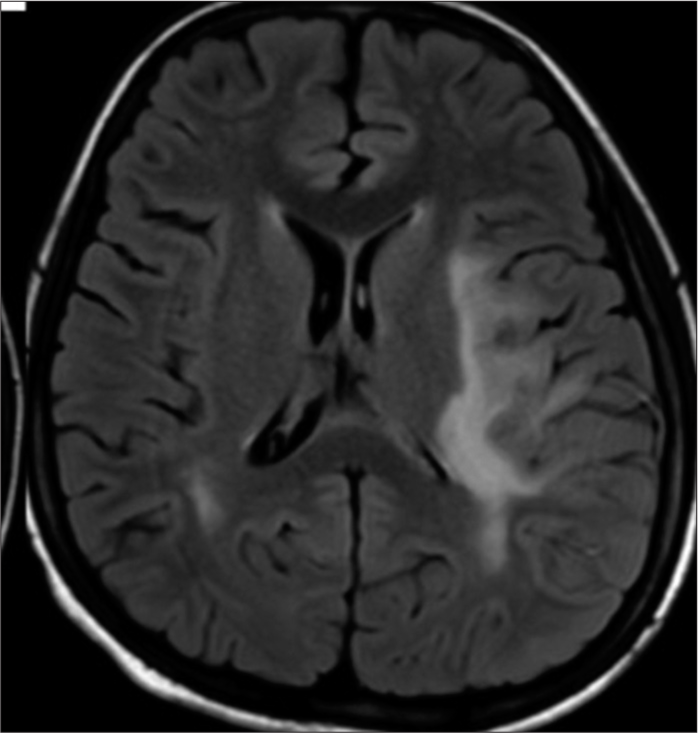
- Axial fluid-attenuated inversion recovery extension of perilesional edema into left thalamus and posterior limb of internal capsule.
Diagnosis of systemic lupus erythematous was made in accordance with the American College of Rheumatology (ACR)/European League against Rheumatism (EULAR) criteria as detailed in Table 2.
| Clinical domains | Points | Immunological domains | Points |
|---|---|---|---|
| Constitutional domain | ② | Antiphospholipid antibody domain | |
| Fever | Anticardiolipin Ig G>40 GPL or | 2 | |
| Anti β2GP IgG>40 units or | |||
| Lupus anticoagulant | |||
| Cutaneous domain | Complement proteins domains | ||
| 1. Nonscarring alopecia | 2 | 1. Low C3 or low C4 | 3 |
| 2. Oral ulcers | 2 | 2. Low C3 and low C4 | ④ |
| 3. Subacute cutaneous or discoid lupus | ④ | ||
| 4. Acute cutaneous lupus | 6 | ||
| Arthritis domain | Highly specific antibodies domain | ||
| Synovitis in at least 2 joints or tenderness in at least 2 joints and at least 30 min of morning stiffness | 6 | 1. Anti ds DNA antibody | 6 |
| 2. Anti -Smith antibody | 6 | ||
| Neurological domain | |||
| 1. Delirium | 2 | ||
| 2. Psychosis | 3 | ||
| 3. Seizure | ⑤ | ||
| Serositis domain | |||
| 1. Pleural or pericardial effusion | 5 | ||
| 2. Acute pericarditis | 6 | ||
| Hematologic domain | |||
| 1. Leukopenia | 3 | ||
| 2. Thrombocytopenia | 4 | ||
| 3. Autoimmune hemolysis | ④ | ||
| Renal domain | |||
| 1. Proteinuria>0.5 g/24 hr | 4 | ||
| 2. Class II or V lupus nephritis | 8 | ||
| 3. Class III or IV lupus nephritis | 10 |
GPL: IgG phospholipid units (1 GPL is equal to 1 microgram of IgG antibody). According to American college of Rheumatology/European League against Rheumatism criteria our patient score was 25. The positive findings were circled.
This child had a score of 25 ( > 10 diagnostic). Renal function tests along with a 24-h urine protein test were normal.
During the hospital stay, child developed abnormal aggressive behavior for which antipsychotic medications were started.
Injection methylprednisolone was administered for 5 days, followed by a single dose of injection cyclophosphamide. Neuropsychiatric complaints improved, no further episodes of seizures were seen, and the patient was discharged on oral steroids (60 mg/m2), tablet hydroxychloroquine, and tablet levetiracetam. In addition, planned for monthly injections of cyclophosphamide for a duration of 6 months. The parents were counseled regarding the disease and the necessity of follow-up.
DISCUSSION
SLE is a multisystemic autoimmune disease with a variety of clinical manifestations and several immune-mediated abnormalities leading to multiple organ dysfunctions. In adult-onset SLE, neurological symptoms and polyarthritis predominate, whereas in children and adolescents, lupus nephritis, hematological disorders, photosensitivity, butterfly rash, and mucosal ulceration are more common.[2] Neuropsychiatric SLE (NPSLE) comprises the neurologic and psychiatric manifestations of SLE in which other causes have been excluded. Although reported in up to 40% adults with SLE, neuropsychiatric involvement is rare in children, especially as initial presentation. A variety of neuropsychiatric manifestations have been described with SLE and have been classified into 19 syndromes in accordance with the ACR, divided into central and peripheral syndromes[3,4] [Table 3].
| Peripheral NPSLE | Central NPSLE | |
|---|---|---|
| Focal | Diffuse | |
| Autonomic disorder | Aseptic meningitis | Acute confusional state |
| Cranial neuropathy | Cerebrovascular disease | Anxiety |
| Mononeuropathy | Demyelinating syndromes | Cognitive dysfunction |
| Plexopathy | Movement disorder/Chorea | Headache |
| Polyneuropathy | Myelopathy | Mood disorder |
| Acute inflammatory demyelinating polyradiculopathy | Seizures | Psychosis |
NPSLE: Neuropsychiatric systemic lupus erythematosus
The NPSLE is mainly clinical, based on the EULAR criteria, supported by MRI findings if present. The neuroimaging findings of NPSLE may result from many different pathophysiologic mechanisms such as vasculitis and vasculopathy, thromboembolic, antiphospholipid syndrome, demyelinating syndrome, and autoimmune antibody-mediated encephalitis.[5,6]
The initial management of NPSLE is focused on symptomatic treatment such as antiepileptics for seizures, anxiolytics or antipsychotics for psychiatric manifestations, antihypertensive drugs for hypertension, and correction of metabolic derangements. In addition, the underlying SLE process of neuropsychiatric manifestations should also be halted, such as thromboembolic disorder and inflammation-driven syndromes with immunosuppressive drugs.[7,8] Studies of NPSLE in adults have shown that treatment regimens including cyclophosphamide in addition to prednisolone and hydroxyurea are associated with better patient outcomes. Other drugs used in this context are mycophenolate mofetil (MMF), azathioprine, and rituximab.[9] Studies on the outcome of children with neuropsychiatric symptoms show that 20% of children experience a disease flare during childhood and 25% may experience a permanent neuropsychiatric damage[10] [Figure 7].
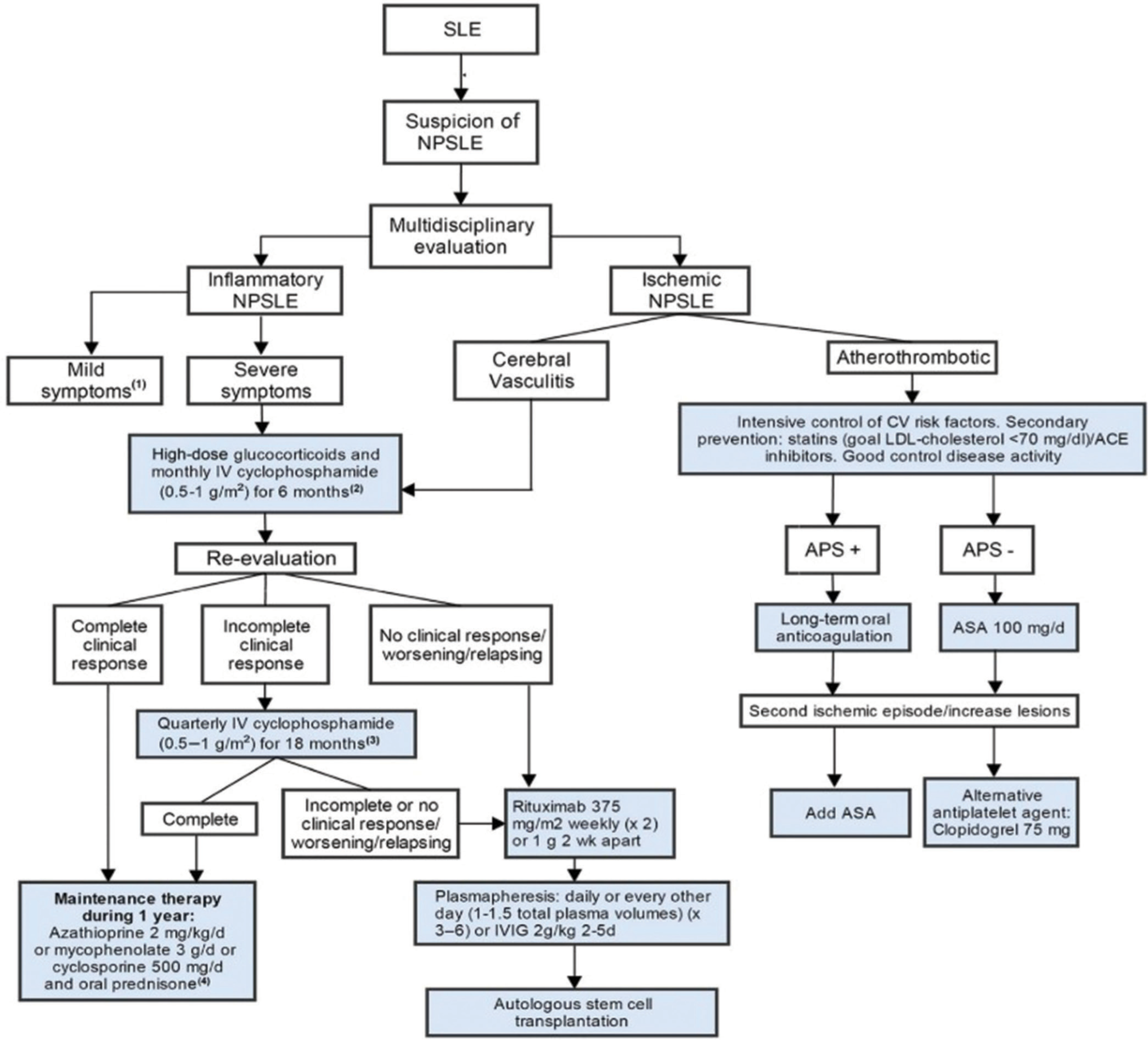
- Management of neuropsychiatric systemic lupus erythematosus. SLE: Systemic lupus erythematosus, NPSLE: Neuropsychiatric systemic lupus erythematosus, IV: Intravenous, CV: Cardio vascular, LDL: Low density lipoprotein, ACE: Angiotensin converting enzyme, ASA: Acetyi salicylic acid, APS: Antiphospholipid syndrome, IVIG: Intravenous immunoglobulin.
CONCLUSION
The clinical spectrum of CNS lupus encompasses various neuropsychiatric manifestations, including cognitive dysfunction, mood disorders, headaches, seizures, psychosis, and cerebrovascular events. These manifestations result from a complex interplay of immune-mediated inflammation, vascular damage, and neuronal dysfunction. The backbone of treatment in NPSLE is steroids and cyclophosphamide.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neuropsychiatric systemic lupus erythematosus in children. Pediatr Ann. 2015;44:e153-8.
- [CrossRef] [PubMed] [Google Scholar]
- Similarities and differences between pediatric and adult patients with systemic lupus erythematosus. Lupus. 2015;24:796-803.
- [CrossRef] [PubMed] [Google Scholar]
- The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999;42:599-608.
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychiatric involvement in systemic lupus erythematosus: A review. Autoimmun Rev. 2021;20:102780.
- [CrossRef] [PubMed] [Google Scholar]
- Review: Nervous system disease in systemic lupus erythematosus: Current status and future directions. Arthritis Rheumatol. 2019;71:33-42.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers for CNS involvement in pediatric lupus. Biomark Med. 2015;9:545-58.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and clinical management of the neuropsychiatric manifestations of lupus. J Autoimmun. 2016;74:41-72.
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychiatric systemic lupus erythematosus: A 2021 update on diagnosis, management, and current challenges. Cureus. 2021;13:e17969.
- [CrossRef] [Google Scholar]
- Neuropsychiatric involvement in pediatric systemic lupus erythematosus. Lupus. 2007;16:564-71.
- [CrossRef] [PubMed] [Google Scholar]
- Management of neuropsychiatric systemic lupus erythematosus: Current approaches and future perspectives. Drugs. 2016;76:459-83.
- [CrossRef] [PubMed] [Google Scholar]






